6 Main Causes of Morning Back Pain
Why is back pain worst first thing in the morning, and what can you do about it?
“I woke up with it” is an amazingly common description of how low back pain started. (And neck pain, and headaches, and even more.1)
Why? Is sleeping dangerous? Probably not: waking up with back pain rarely indicates a serious problem. But both mornings and backs are unusually vulnerable to some common minor sources of pain.
This is mostly about chronic back pain that’s at its worst in the morning, a common pattern. Even many people who are more or less pain-free during the day may still experience routine and significant irritation and stiffness first thing in the morning. But attacks of acute back pain are also much more common in the first few hours of the day,2 and that phenomenon may be related to why chronic back pain tends to be bad in the morning.
Morning back pain is a tough problem to treat because most of it probably has several subtle chronic causes, but there may be some opportunities for treatment.

Is pain & stiffness your alarm clock? Do you bail out of bed early every morning with low back pain, neck pain & more?
The 6 big causes of morning back pain
- Inflammatory back pain: pathological inflammation from autoimmune disease, which is often serious, relatively rare, and fairly well known.
- “Inflammaging”: slow but steady increase in chronic mild inflammation as we age.
- Myofascial pain syndrome and/or fibromyalgia: back pain is often the hot spot in the body for muscle pain and otherwise unexplained widespread aches and pains, and there are some reasons why these conditions may be worse in the morning, but they are mysterious and controversial.
- Insomnia and poor quality sleep is, of course, the most basic explanation for morning back pain. A good night of sleep is an effective painkiller, and a lousy one is the opposite.
- Osteomalacia (vitamin D deficiency): vitamin D deficiency is probably quite common, is linked to chronic pain, and morning bone aching in particular.
- Awkward sleeping postures: although this is the most “obvious” reason for waking up with a kink in your back, it might be worse than you expect.
3 myths about the causes of morning back pain
There are some popular ideas about what causes back pain that are probably wrong (or at least a lot more rare and trivial than believed):
- Bad mattresses are generally over-rated as a factor in back pain.
- Psychological factors are also often given too much weight. The mind is relevant to a lot of chronic pain, but morning back pain is particularly unlikely to be psychosomatic.
- Intervertebral disc swelling is a popular specific scapegoat, but it’s highly speculative and quite likely wrong.
All of these causes are discussed below, along with many treatment options and suggestions. Click the green headings above to jump down to a section.
The scariest type of morning back pain: inflammatory back pain
The closest thing to back pain that is truly prominent in the morning is inflammatory back pain (IBP), or spondyloarthritis.3 Although IBP is well known to medical science, it often eludes diagnosis, its biology is mysterious, and morning symptoms specifically are a stumper, as unexplained as joints that ache before a storm. It’s just something IBP does.
But don’t panic! Although studies have confirmed that morning is a common time for inflammatory back pain to flare up, they have also shown that the connection is not strong or exclusive.4 In fact, most morning stiffness and pain is not pathologically inflammatory. It’s just that IBP is the only “official” morning back pain culprit.
The pain of IBP tends to be quite severe. If it’s not actually waking you up, it’s probably not IBP, or it’s a minor case.
When should you consider the possibility of IBP? Basically if your morning back is particularly bad: nasty and very consistent morning symptoms. The diagnosis is also more likely if you have other signs of this kind of back pain. Here’s a good inflammatory back pain quiz, and here’s my own quick checklist of reasons to ask your doctor about spondyloarthritis:5
- signs of inflammation in other body parts, especially tendons (where they attach to bone), eyes, fingers or toes, colon
- a family history of spondyloarthritis (although it develops slowly, it’s a serious disease, so you’ll definitely know if someone in your family had it), or other autoimmmune diseases
- you respond fairly well to NSAIDs (Aspirin, Ibuprofen, etc)
- an infection in the weeks before your back trouble began
Technically IBP causes night back pain, not morning back pain
The morning pain of IBP is actually a case of leftover nighttime symptoms, which wear off as you wake up and get moving. When the symptoms are milder, you will mostly sleep through them, noticing them only when you wake up. But these symptoms will usually be obvious while you are still in bed, as soon as you are conscious — or even waking you up early.
In contrast, pain that you don’t notice until you actually get up and start trying to move around is less likely to be inflammatory in nature. But these are rules of thumb only, of course — there’s always lots of exceptions in biology.
PATIENT: Doctor, my back hurts when I wake up in the morning.
DOCTOR: Wake up in the afternoon then.
Doctors, do not actually trying giving this advice with patients! Joke (with visuals) via 9GAG with a hojillion likes and shares on Facebook.
•
Myofascial pain syndrome and/or fibromyalgia
There are two common types of widespread moderate body pain, both somewhat mysterious and controversial, both known for affecting the back more than other areas, and both known for their morning hijinks:
- Myofascial pain syndrome (MPS) is an infestation of too many “trigger points” — sore, aching patches of soft tissue that often seem to ease with massage and heat, but which are mostly unexplained and difficult to treat.
- Fibromyalgia (FM), a disease of increased soreness and sensitivity, fatigue, and sleep disturbance, exercise intolerance, and the infamous “fibro fog” (mental confusion).
There’s likely lots of overlap between these conditions. Fibromyalgia isn’t really an explanatory diagnosis; it just labels a common pattern of symptoms that probably have different causes in different people. MPS is a hypothetical problem with muscle tissue that is a possible explanation for some body pain, and that type of pain is extremely common in fibromyalgia patients.
Fibromyalgia is associated with morning back pain because:
- People with FM rarely feel rested. The condition either causes or is caused by fragmented sleep and a lack of deep restorative sleep. Fatigue makes any pain worse, and this is probably felt mostly acutely in the morning, gradually (and imperfectly) yielding to the stimulations of the day: exercise, sunlight, coffee, people, noise and so on. The morning-ness of fibromyalgia pain could also just be “one of those things,” an unexplained rhythm of the disease.
- Although FM involves widespread pain by definition, back pain is a routine hot spot.
And trigger points may be associated with morning back pain because:
- Tissue stagnancy and postural stress seem to be a major cause of flare ups of pain of this kind, and both are an issue at night: we are often pretzeled into awkward positions in our sleep for long periods.
- The paraspinal muscles seem to be particularly vulnerable to trigger points. Whatever they are, they happen more in those muscles (and a few others).
The tendency of FM and MPS to affect the back in particular might be because they each affect it in their own special nasty way, or it could be two sides of the same coin. Perhaps fibromyalgia affects the back more than other areas because it causes vulnerability to trigger points … which seem to occur in the back muscles much more than other muscles.6
Fibromyalgia and MPS both exist on a wide spectrum of severity. Fibromyalgia’s diagnostic criteria are notoriously tricky.8 MPS is barely even recognized as a clinical entity. Many people may have mild cases that will never be diagnosed, but morning back pain may be the tip of that iceberg — the most likely time and place for the symptoms to be felt, even if you are otherwise mostly fine.
What do you do about trigger points and fibromyalgia?
Those are both big, separate topics, but there are many resources on PainScience.com where you can get started. Self-massage and heating are by far the best (cheap, safe) ways to start working on muscle knots. Fibromyalgia is much more complicated, but the basics are sleep improvements, lots of light but thorough exercise, and learning about sensitization and the weirdness of pain.
•
Chronic low-grade inflammation and “inflammaging”
Everyone over 40 knows that it gets more uncomfortable to get out of bed as we age. Most people chalk it up to “arthritis,” but that’s rarely a significant factor until much later in life. Conditions like fibromyalgia and myofascial pain syndrome, as common as they are, can’t account for all of it. So what’s the problem?
A little bit of inflammation spread all over the place is a likely culprit. This might happen as a consequence of “metabolic syndrome,” a set of biological dysfunctions strongly linked to poor fitness, obesity, and aging, and possibly linked to severe chronic stress as well.9
And aging itself seems to be inflammatory (no matter how fit, skinny, and calm you are), which is known as “inflammaging.”10 So, if you’re on the far side of middle age, or you’re younger but struggling with your weight and/or major long-term stress, chronic inflammation could be your issue.
Connecting inflammaging to the curse of morning back pain
This inflammaging thing is intriguing, but does it have anything to do with morning pain or back pain specifically?
The morning link isn’t much of a reach: for whatever reason, inflammatory diseases are notoriously morning-o-centric (like the more serious inflammatory back pain mentioned above), and so it’s reasonable to assume that less serious inflammation has a thing for the morning too. We also know — only just recently — that the body can suppress inflammation at night, pumping out an anti-inflammatory protein on a schedule,11 which probably accounts for some morning pain and stiffness as the suppression wears off. No one knows anything about how to actually control that effect, but at least we know it exists.
The back link is trickier. Being overweight is less of a risk factor for back pain than most people think,12 so there’s no obvious association with metabolic syndrome. If there is a connection, it might be that the spinal joints are among the first structures to be affected by inflammation — and not necessarily because they are more fragile or harder working than, say, knees, but perhaps because the brain seems to be quite over-protective about the back, and more likely to raise the alarm sooner, louder, and longer.
Also, we do know that metabolic syndrome is associated with at least some common pain problems, like neck pain.13
It could also just be simple overlap: maybe these problems often just all happen at once. Inflammaging gets to everyone sooner or later, and back pain is spectacularly common, so they probably co-exist in the same people whether they have anything to do with each other or not.
How do you treat inflammaging? Lifestyle medicine
No one really knows, but it’s probably all about just being as fit and healthy as possible, and reducing biological vulnerabilities (also known as “lifestyle medicine”). Systemic inflammation is almost synonymous with being out of shape — and all the bad habits that tend to go with it — so these very general approaches to health can be considered “inflammation treatments” specifically. But they are also a sensible everything-but-the-kitchen-sink approach to treating any health problem we don’t understand (which is why this list overlaps a lot with fibromyalgia treatment).
Their superpower is that it’s hard to actually waste your time doing this stuff. It’s all good for you, whether it helps morning back pain or not.
- Get more exercise. It’s the closest thing there is to a miracle drug. Building strength is really valuable and surprisingly efficient.
- Get more sleep. Protecting your sleep is probably almost as good an investment as exercise.
- Eat an “anti-inflammatory diet” — which is just healthy! It’s more about avoiding dietary causes of inflammation (junk food and excess, basically) rather than consuming anything “medicinal.” (The omega-3 fatty acids — fish, nuts — are by far the best example of nutrition that verges on medicinal. Everyone should probably eat more mackerel.) Intermittent fasting (skipping some meals) is an approach, overhyped but probably based on a seed of truth.
- Inhale less smoke. If you smoke, you already know you should quit, of course. And now that COVID-19 is rampaging around the world, you have the best reason yet.
- Drink less alcohol. Alcohol is a poison, and the more you drink, the harder it is on your system. (Moderate drinking is pretty harmless, but the popular idea that it’s actually “healthy” is nonsense.)
- De-stress. The ultimate easier-said-than-done challenge! If you are a candidate for an anxiety disorder diagnosis, exploring and treating that should probably be your top priority.
- Make more friends. “Loneliness” is an incredibly common and underestimated stressor.
What about more specific inflammation treatments? There are many. Obviously there are OTC anti-inflammatory drugs. They aren’t a long-term solution — those drugs are too hard on the GI tract for anything but taking the edge off now and then. But they might do that, and if they do it’s also good diagnostic evidence that the issue is caused by inflammation. Inflammation can also be nuked by some more potent drug therapies, but those “cures” are definitely worse than the disease of morning back pain.
I have an article specifically about inflammation that goes into more detail about managing inflammation:
•
Poor quality sleep and insomnia are probably major causes of morning back pain
Don’t get me wrong: some people sleep just fine and still have morning back pain. But poor quality sleep and pain definitely tend to go together,14 and mornings can be the roughest part of that link.
The more interesting question is the chicken/egg thing: which comes first? Pain or sleeplessness? Once you have both insomnia and pain, they surely cause each other, but one side of that equation is probably more important than the other, like a cyclist pushing much harder on one pedal than the other.
In 2017, Gerhart et al studied the which-came-first question of pain and insomnia in 105 chronic low back pain patients.15 Their subjects bravely filled out five detailed questionnaires per day for two weeks — that’s a lot of paperwork! — tracking and rating many aspects of their pain and sleep quality. The goal was to study “lagged temporal associations”: what tends to happen after what? Are bad sleeps often followed by bad days with back pain? Are rough days with back pain followed by lousy sleeps?
Yes and no to those two questions.
The relationship did not flow the other way. That is, bad nights were likely to be followed by bad days… but bad days were not followed by bad nights. The data shines a nice bright light on a simple old question. The answer isn’t much of a shock to anyone who struggles with both back pain and insomnia, but it’s important and rare to confirm this stuff with a good study.
And it gives us a compelling incentive for focussing on sleep quality as a major factor in pain generally, especially morning back pain. And almost everyone can benefit in many ways from upgrading their sleep quality. To drive that home, let’s take a closer look at the biology…
Inflammation, sleep, stress, and pain
The link between sleep and pain is based on some superficially simple inflammatory biology: bad sleep is inflammatory… and inflammation makes it harder to sleep, which is not widely appreciated. That means that sleeping badly can actually make it harder to sleep well!16 This is a vicious cycle every extremely frustrated insomniac is familiar with: being exhausted from a sleepless night is not a guarantee that you will sleep well the next night.
And that vicious cycle is relevant to night and morning pain, which is known to be significantly mediated by the immune system signalling molecule interleukin-6. IL-6 and inflammation are almost synonymous — more of one means more of the other. Everyone knows that stress makes it harder to sleep, but how? It’s not just because your mind is racing — it’s because stress makes us produce IL-6, which is inflammatory, and inflammation in turn makes it harder to sleep! And then the bad sleep also makes us pump more IL-6…
And that’s why it’s important to get your sleep!
•
Osteomalacia (Vitamin D deficiency)
Vitamin D deficiency is probably more common than once suspected — at least 1 in 20 people in the lowest estimates,17 and possibly many more.18 Vitamin D deficiency can cause subtle widespread pain that may be misdiagnosed as fibromyalgia and/or chronic fatigue syndrome. Most notably for the purposes of this article, it can cause bone aching, particularly in the back, that is worse at night (for no clear reason). Naturally, any night pain that doesn’t actually wake you up is often noticed upon waking.
This symptom is caused by osteomalacia, which is bone weakening from malfunctioning bone building biology. The Mayo Clinic describes osteomalacia symptoms like so: “The dull, aching pain associated with osteomalacia most commonly affects the lower back, pelvis, hips, legs and ribs. The pain may be worse at night, or when you’re putting weight on affected bones.”
Other symptoms of vitamin D deficiency include: fatigue and weakness, lower pain threshold, and more acute soreness after exercise that is slower to resolve, sweating, and depression. For more information, see Vitamin D for Pain.
•
Awkward sleep postures
In 2015, Steffens et al found that most “back attacks” — episodes of acute back pain — occur in the first few hours of the day.19 They also identified an “awkward posture” in the two hours preceeding the attack as the second biggest risk factor (after “distracted during an activity”). Although their study wasn’t perfect, the results were too strong not to take seriously. Notably, just an “awkward posture” was quite a bit more likely to be associated with acute back pain than much more traditional bogeymen like difficult or sloppy lifting.
Based on this evidence, we could surmise that morning back pain might be so common because sleeping is a rich source of awkward postures. In people with chronic back pain especially, it may be a routine source of minor irritation of their ongoing problems.
Awkward positions can be quite painful, even injurious. Sleeping often involves slightly awkward positions held long enough to cause sustained compression, pinching, and oxygen starvation of tissues (which may or may not have been vulnerable or irritated to begin with). The dose makes the poison: it doesn’t have to be a terrible spine position to cause trouble. Just a little awkwardness will do the job if you’re stuck that way for long enough. Although people can also carelessly tolerate postural stresses while wide awake — we generally move before they become a problem — it’s much more of a risk at night.
Sooner or later, any posture gets awkward — the trouble with tissue stagnacy regardless of position
Being still always gets uncomfortable, regardless of what position we’re in. We like to move, and sitting or lying down always gets uncomfortable in time. Forced immobilization is a potent torture method. Working in stagnant postures — like sitting in at a desk, no matter how well we do it — can start to feel more like a kind of torture as we age.20
Sleeping is an obvious potential source of tissue stagnancy, of course, but beds are more comfortable than chairs in every way, physically and psychologically. Healthy young people are relatively immune to simply being still in bed, but as we age and develop assorted vulnerabilities and sensitivities — things like fibromyalgia, myofascial pain syndrome, and chronic inflammation — it starts to become a problem.
Trigger points may be aggravated by stillness, for instance.21 Morning pain could be a wake-up call (ha ha), letting you know that you have a bumper crop of mostly asymptomatic (“latent”) trigger points that flare up overnight. In Lita’s case, trigger points could account for the consistency of her symptom timing, and for the peculiar way in which she is fine at 6am, yet can’t stay in bed past 7am, but then is fine again by 8am as she gets moving and her trigger points calm down.
Minor injury (or re-injury)
We may also cause minor injuries in our sleep, or aggravate existing minor injuries and vulnerabilities (like chronic minor back pain). Sometimes you just roll over and pinch something hard enough and quickly enough to hurt it — maybe not even enough to wake you up, but enough to feel the consequences when you do wake up. Usually this is going to be an isolated incident, but what if you keep pissing off the same vulnerable tissue?
For instance, suppose you already have minor intermittent back pain related to an old accident: it’s bothered you for years, off and on, and you’ve learned that leaning backwards is usually bad news. But then you do it in the middle of the night in your sleep, an extended lumbar spine for an hour when you weren’t even conscious — no fair! And so you wake up in moderate pain.
In other words, whatever is bothering your back in the first place can be easily and routinely aggravated — re-injured — by common sleeping positions.
I have no personal experience with back pain like this, but I know exactly what this is like from trying to sleep with a shoulder injury.22
Such incidents won’t explain all chronic, consistent morning back pain, because you’re unlikely to slightly but frequently re-injure yourself in the same way. Or maybe it’s not so unlikely: if bending your spine one way or the other is a problem, it might be easily avoided during the day, but happen to some degree most nights. Again, it’s the duration that’s the issue.
Is there such a thing as “poor posture” when sleeping?
Yes, but I believe it’s relatively rare for it to be bad enough to matter much. As discussed already, most awkward postures during sleep involve relatively minor postural stresses — being a little twisted this-a-way or that-a-way — that we tolerate for too long because we’re unconscious. Such postural stresses aren’t a bad habit in any meaningful sense. But it is also possible to be so habitually careless with sleeping position that it does constitute “poor posture.” If you know that a particular sleeping position is uncomfortable for you, but you keep sleeping like that, that’s a “poor” sleeping posture. 😉
Or is it a bad habit if you can’t stop it? If it’s something you do “habitually” but unconsciously? This is a philosophical puzzle for the reader to work out.
Habitual sleeping position is clearly a factor in some back pain. Just about the only study ever done on this topic showed a small improvement in a few back pain patients who were “instructed regarding the recommended way to sleep” — which basically meant a more neutral position.23 The benefit was real but small. I think conscious sleep positioning is only a minor factor in low back pain, and tough to fix. Usually we don’t even suspect a problem with our sleep posture until it’s too late! For most people, trying to work on sleeping position probably does not offer particularly good bang for buck.
The most likely habitual position to cause trouble is face down.
We can do a little to minimize the chances of an awkward position, mainly by starting out as comfortably as we can, and adding a little bracing with pillows to discourage too much rolling around. Using a knee pillow is the best example of this: just put an extra pillow between your knees while lying on your side. This reduces rotation in the spine, and rolling face down. Unfortunately, most people who toss and turn can make short work of any pillow arrangement in their sleep. Any pillow that’s in my way is kicked off the bed in about five minutes.
•
Mattress and pillow changes and upgrades
Mattresses are touted as both cause and cure of morning back pain. As a cause, they allegedly constitute a significant source of postural stress — basically, the idea is that you have poor sleeping posture because of a mattress. This is all a more specific version of the topic of posture, but it is the most significant and popular version.
I have no doubt that there are mattresses that are bad enough to cause trouble. What I doubt is that there are mattresses that basically seem fine, and yet still cause this serious chronic symptom. In other words, if the problem is the mattress, it’s probably obvious that the mattress is uncomfortable; and if the mattress isn’t obviously uncomfortable, it’s probably not causing significant morning back pain. I doubt there’s a large ambiguous sweet spot between those, where large numbers of people are being plagued enough for it to be a problem, but not enough that it’s obvious why.
The world is stuffed with claims about better mattresses and pillows, and you can even find the extreme opinion that we should get rid of them entirely and sleep on the ground, “naturally” — paleo sleeping!24 🙄 But even the tamest of these claims are wishful thinking.
Comfort is a critical factor, and there are so many subjective variables in what constitutes “comfortable” that it is impossible to objectively define a “best” mattress or pillow. Oddly, it’s also actually impossible to really know our own preferences! We really can’t know how comfortable a mattress is without sleeping on it for a couple weeks. We’d have to buy a series of mattresses and take some really careful notes on sleep quality, and even that would be imperfect. Testing pillows is more practical, but not much.25
There is a bit of evidence that a new mattress can improve back pain.26 A small study found that back pain was worse for people with the cheapest and oldest mattresses, and improved when they got better new mattresses. The difference was not dramatic, but worth noting, and undoubtedly worthwhile. If insomnia or the sleep disturbances of fibromyalgia are part of your problem, it’s probably a good idea to optimize anything you can.
The anti-nap: take a sleep break
Here’s one weird, good trick, mostly a way to help with nightime postural stress: if you’re really struggling with night and morning pain, break up the night. Just like you need breaks from long stretches of sitting, you may need to take a break from sleeping.
If you’re actually sleepless and in pain, don’t stay in bed squirming in misery all night — get up and help yourself! Or if you are sleeping, set an alarm! Either way, get out of bed, and mobilizations, heating, or self-massage your back — or whatever else you’ve ever found helpful. Or ignore your back and do something pleasant.
If you were in an awkward position when the alarm went off, you may really be doing yourself a favour by interrupting it. You can “reset” your sleeping position when you go back to bed.
Few people have ever thought of trying this, let alone taken it seriously, or tried it consistently for a few nights. There’s an understandable emotional reluctance to interrupting sleep for the sake of doing therapy on yourself — we’re all over-tired, and that’s an issue too — but it may well be the lesser of evils, if sleeping is hurting your back.
Stranger still, it may even be unhealthy (as well as painful) to try to sleep all the way through every night. There is actually a natural wakeful period in the middle of the night, like a mirror image of afternoon naps, which most modern people are resisting — we think we’re supposed to be asleep all night!27 But that natural tendency to wake up for a bit may actually exist to prevent excessive tissue stagnancy! So try not fighting it for a while — you don’t have to do it every night, or forever. If it helps you get through a rough patch with your back, it’s certainly worth a shot. And it’s worthwhile if it helps you sleep when you go back to bed!
Final tip: try getting up and taking care of your back for a few minutes without turning on a light — staying in the dark will help preserve “sleep mode.”
•
Are there psychological factors that drive morning pain?
Probably not. The book Back Sense proposes that morning back pain is caused by “stressful night-time mental patterns manifesting as back pain.” I do not dismiss the role of psychology in back pain — quite the opposite! it’s a major theme in my writing about back pain. See The Mind Game in Low Back Pain.
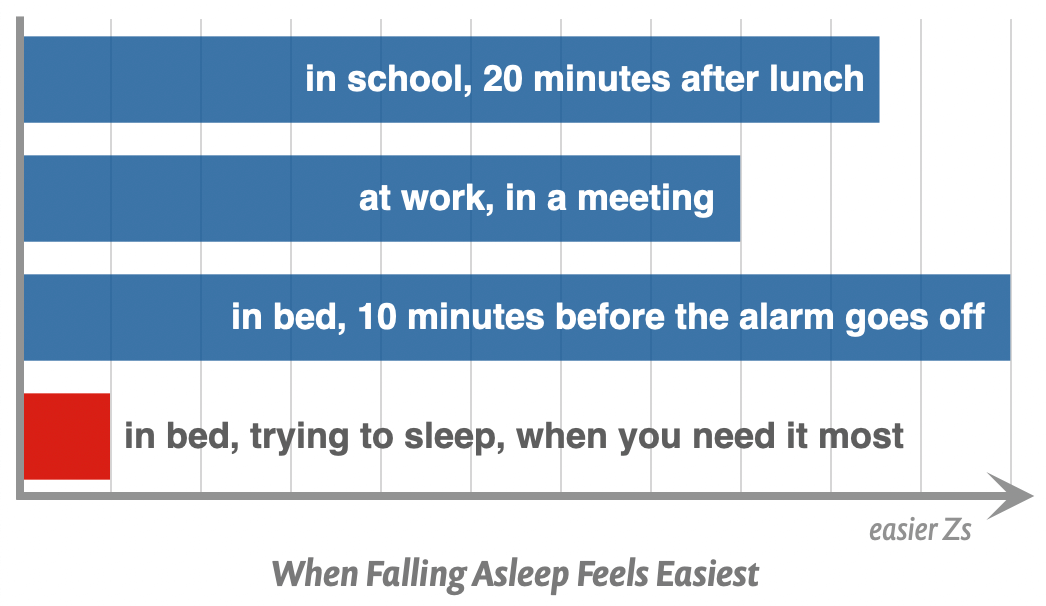
But I think that author is indulging in a simplistic mind-body connection theory. I’ve written crankily about this kind of logic elsewhere (see Why Do We Get Sick? or Mind Over Pain). It’s a bit of a reach to say that you have such a problematic, pain-causing mental state like clockwork every morning between 6am and 7am exclusively. Applying How to Simplify Chronic Pain Puzzles to the problem, it is much (much!) more likely that there is simply a time limit on how long you can lie in bed without tissue crankiness.
•
What about nocturnal intervertebral disc swelling?
The last two sections of this article are reserved for PainSci members: one interesting, one useful. Just a little bonus content, about 600 words in all.
- What about nocturnal intervertebral disc swelling?
- Morning baths are almost miraculous for some kinds of morning back pain
These are also available in my back pain book ❐, which has a substantial free introduction. To access this content, please buy a membership (or the book).
Most PainScience.com content is free and always will be.? Membership unlocks extra content like this for USD $5/month, and includes much more:
Almost everything on PainScience.com is free, including most blog posts, hundreds of articles, and large parts of articles that have member-areas. Member areas typically contain content that is interesting but less essential — dorky digressions, and extra detail that any keen reader would enjoy, but which the average visitor can take or leave.
PainScience.com is 100% reader-supported by memberships, book sales, and donations. That’s what keep the lights on and allow me to publish everything else (without ads).
- → access to many members-only sections of articles +
And more coming. This is a new program as of late 2021. I have created twelve large members-only areas so far — about 40,000 words, a small book’s worth. Articles with large chunks of exclusive content are:
- Quite a Stretch
- Does Epsom Salt Work?
- Heat for Pain and Rehab
- Your Back Is Not Out of Alignment
- Trigger Point Doubts
- Does Fascia Matter?
- Anxiety & Chronic Pain
- A Deep Dive into Delayed-Onset Muscle Soreness
- A Painful Biological Glitch that Causes Pointless Inflammation
- Guide to Repetitive Strain Injuries
- Chronic, Subtle, Systemic Inflammation
- Reviews of Pain Professions
- Articles with smaller members sections (more still being added):
- → audio versions of many articles +
There are audio versions of seven classic, big PainSci articles, which are available to both members and e-boxed set customers, or on request for visually impaired visitors, email me. See the Audio page. ❐
I also started recording audio versions of some blog posts for members in early 2022. These are shorter, and will soon greatly outnumber the audio versions of the featured articles.
- → premium subscription to the PainSci Updates newsletter +Sign-up to get the salamander in your inbox, 0–5 posts per week, mostly short, sometimes huge. You can sign-up for free and get most of them; members get more and their own RSS feed. The blog has existed for well over a decade now, and there are over a thousand posts in the library. ❐

Pause, cancel, or switch plans at any time. Payment data handled safely by Stripe.com. More about security & privacy. PainScience.com is a small publisher in Vancouver, Canada, since 2001. 🇨🇦
The salamander’s domain is for people who are serious about this subject matter. If you are serious — mostly professionals, of course, but many keen patients also sign-up — please support this kind of user-friendly, science-centric journalism. For more information, see the membership page. ❐
This is one of the classic theories about why people seem to be more vulnerable to back pain in the morning. Unfortunately, it’s too speculative to be really satisfying. But what’s the speculation?
Between every pair of vertebrae is a bit of padding, the infamous disc. They probably swell up a wee bit overnight. There are two studies that suggest this2829 (although one of them was a study of long term bed rest, and only barely applicable here). A 2016 paper speculates that disc swelling is why astronauts probably suffer from more disc herniations than they should.30 Weightlessness is undoubtedly like resting your spine, but it’s another long-term effect, so I’m not sure how relevant the astronaut angle is — it’s just a fun angle on the topic.
Discs may swell, but that doesn’t mean swelling discs hurt. Mild swelling is hardly a concern in itself, and most people don’t wake up in pain, so it’s unlikely that swelling alone is a problem. Swollen discs may hurt more in the morning if there’s already something wrong with them, such as annular tears,31 but such discs might well be uncomfortable regardless. Mildly herniated discs might swell and effectively be more herniated in the morning — but many herniations are painless, so that’s hardly a smoking gun.
It’s an interesting possibility that nocturnal disc swelling is a factor in morning back pain, but the truth is beyond our reach. For all we know, problems with discs might be much more aggravated by postural stress … or it could be a complicated combination, such as swelling that is exaggerated by postural stress but still only hurting when other problems are present.
Morning baths are almost miraculous for some kinds of morning back pain
A hot bath is one of the oldest medicines. While most people appreciate a nice hot bath, few people think of it as a serious treatment for back pain — just something that takes the edge off. Maybe.
But for morning back pain, it can be incredibly effective. Reader C.B. writes:
I am 73 with assorted age-related issues, but this low back pain every morning is new. Here is what I do: I run a hot bath, and jump in and immediately the pain goes away, all of it. Why would that be, and what does it mean?
C. is not alone: many people report near rapid, profound relief from morning back pain. Baths seem to be at their best in this context, and it’s not clear why. When a bath has an immediate, profound effect on pain, it’s probably because immersion/flotation is a fairly potent dose of “novel sensory input,” which can very persuasively tell the brain that there’s no need for the alarm of pain. This may be more pronounced with some kinds of pain that are aggravated by gravity, so the partial flotation might be directly relieving.
And then, by the time you get out of the bath, the relatively transient phenomenon of morning back pain is already retreating … and perhaps even faster because of some thermal effects (getting the blood flowing, etc).
But all that’s speculation. No one really knows! It’s not always super convenient to take a bath in the morning, but if you suffer from stubborn morning back pain, it’s worth a try at least some of the time. I’d like to hear more about this from readers: please let me know if hot baths do or don’t help your morning back pain. Believe it or not, I actually have an entire, surprisingly large article about bathing tips. See: Hot Baths for Injury & Pain: Tips for getting the most benefit from a hot soak, the oldest form of therapy.
P.S. Showers may be just as good! Or nearly as good. It would be nice if I could cite a nice, well-controlled trial of this, but that’s probably never going to happen.
↑ MEMBERS-ONLY AREA ↑
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
- Neuropathies Are Overdiagnosed — Our cultural fear of neuropathy, and a story about nerve pain that wasn’t
- Don’t Worry About Lifting Technique — The importance of “lift with your legs, not your back” to prevent back pain and injury has been exaggerated
- Chronic Low Back Pain Is Not So Chronic — The prognosis for chronic low back pain is better than you think
- The Mind Game in Low Back Pain — How back pain is powered by fear and loathing, and greatly helped by rational confidence
- The Tyranny of Yoga and Meditation — Do you really need to try them? How much do they matter for recovery from conditions like low back pain?
- Back Pain & Trigger Points — A quick introduction to the role of trigger points and massage therapy in back pain
- Vulnerability to Chronic Pain — Chronic pain often has more to do with general biological vulnerabilities than specific tissue problems
- Does Posture Matter? — A detailed guide to posture and postural correction strategies (especially why none of it matters very much)
- The Trouble with Chairs — The science of being sedentary and how much it does (or doesn’t) affect your health and back pain
What’s new in this article?
Seventeen updates have been logged for this article since publication (2007). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more
When’s the last time you read a blog post and found a list of many changes made to that page since publication? Like good footnotes, this sets PainScience.com apart from other health websites and blogs. Although footnotes are more useful, the update logs are important. They are “fine print,” but more meaningful than most of the comments that most Internet pages waste pixels on.
I log any change to articles that might be of interest to a keen reader. Complete update logging of all noteworthy improvements to all articles started in 2016. Prior to that, I only logged major updates for the most popular and controversial articles.
See the What’s New? page for updates to all recent site updates.
2020 — New section, “Poor quality sleep and insomnia are probably major causes of morning back pain.” Also made some minor improvements to the introduction and article summary.
2020 — Comprehensive editing. Re-wrote the summary. Refined advice on treating inflammation. Explained fibromyalgia more clearly and accurately. Added more about mattresses. Improved organization, in-document navigation, and added a few sprinkles of humour.
2018 — Significant science update: cited Steffens on back pain risk factors, a fascinating study that adds some important data to this article.
2018 — New section: “Morning baths are almost miraculous for some kinds of morning back pain.”
2017 — Added a mostly amusing footnote about natural sleeping postures or “paleo sleeping” (but worthwhile for perspective).
2017 — Added footnote about the lack of a link between back pain and sitting too much.
2016 — New section about vitamin D deficiency and the nighttime bone pain caused by osteomalacia.
2016 — Added an article summary. Miscellaneous improvements, mainly to the introduction and about fibromyalgia.
2016 — Minor science update: interesting new citation about evidence of inflammation suppression at night (Hand et al).
2016 — Huge upgrade: completely rewrote almost everything about trigger points and added much more about fibromyalgia; revised everything about tissue stagnancy, postural stress, and sleeping position; added an important large new section about inflammation and “inflammaging”; added a minor new section about mattresses; added several more specific tips and suggestions.
2016 — Added some information about fibromyalgia and some other causes of non-back morning pain.
2016 — Edits and elaborations for new nocturnal disc swelling section.
2016 — New section: “What about nocturnal intervertebral disc swelling?”
2016 — More editing, clarifying the idea of postural stress at night: “the dosage makes the poison.”
2016 — Editing for clarity and readability, first half. More information about the vulnerability of the paraspinals to trigger points. New image of a messy bed.
2016 — Major revision: a new structure for the article. It’s now built around three possible causes of morning back pain. Modernization of trigger point information as well.
2016 — An important update: added a whole bunch of new information about inflammatory back pain. Its absence in previous versions of the article was a major oversight.
2007 — Publication.
Notes
Morning pain and stiffness is a symptom of several common conditions, including fibromyalgia, osteoarthritis, rheumatoid arthritis, plantar fasciitis, Achilles tendinitis, and carpal tunnel syndrome. (Most repetitive strain injuries are probably worse in the morning, but it’s more obvious with some than others.)
Most of these do not primarily affect the back, however.
- Steffens D, Ferreira ML, Latimer J, et al. What triggers an episode of acute low back pain? A case-crossover study. Arthritis Care Res (Hoboken). 2015 Mar;67(3):403–10. PubMed 25665074 ❐
This study of triggers for episodes of back pain “brief exposure to a range of physical and psychosocial factors,” mainly being distracted during an activity and awkward postures, can “considerably increase the risk of an episode of acute back pain,” and much more so in the morning:
Mornings were the most frequent time of day for back pain onset, with 35.2% of participants (n=352) reporting pain onset between 7:00 AM and 10:00 AM (Figure 2). Only 3.7% of participants (n=37) reported pain onset between mid- night and 5:00 AM, with a large increase in reports from 6:00 AM.
- IBP and spondyloarthritis are umbrella concepts for several other rheumatic (inflammatory) diseases, including ankylosing spondylitis, reactive arthritis, psoriatic arthritis, inflammatory bowel disease-related arthritis. There are also cases that can’t be classified: “generic” spondyloarthritis. Although it develops slowly, this is one of the rare scary causes of back pain. You don’t want this diagnosis.
- Arnbak 2016, op. cit. 82% of more than 700 patients with chronic low back pain reported “morning stiffness” — practically everyone! — but only 11% actually had spondyloarthritis (according to ASAS criteria). Only 10% felt that their pain was worst in the morning. Although these and other inflammatory back pain signs were significantly associated with spondyloarthritis, there’s just too much overlap with other kinds of back pain for morning symptoms to actually identify spondyloarthritis.
If indicated, a doctor can get you checked out for other signs, like blood tests that show elevated CRP, and/or the presence of a particular gene, HLA-B27. An MRI can also help diagnose this kind of inflammation.
- In my back pain book, I get into some of the possible reasons why trigger points seem to favour the back. No one really knows what it’s about, but it’s certainly a thing. Ask any massage therapist: we get a lot more requests for back massage than, say, upper arm or abdominal massage.
- Ablin JN, Eshed I, Berman M, et al. Prevalence of axial spondyloarthropathy among patients suffering from Fibromyalgia - an MRI study with application of the ASAS classification criteria. Arthritis Care Res (Hoboken). 2016 Jul. PubMed 27390225 ❐
- www.rheumatologynetwork.com [Internet]. Garg N. New and Modified Fibromyalgia Diagnostic Criteria; 2016 August 24 [cited 20 Jul 24]. PainSci Bibliography 53279 ❐
An excellent explanation (for professionals) of the changes in diagnostic criteria for fibromyalgia. See also Wolfe).
- Prolonged chronic stress can probably contribute to metabolic syndrome (Gohil et al) by messing with the hormonal balance of the hypothalamic-pituitary-adrenal axis (HPA-axis).
- Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014 Jun;69 Suppl 1:S4–9. PubMed 24833586 ❐ PainSci Bibliography 53291 ❐ “Human aging is characterized by a chronic, low-grade inflammation, and this phenomenon has been termed as "inflammaging." Inflammaging is a highly significant risk factor for both morbidity and mortality in elderly people, as most if not all age-related diseases share an inflammatory pathogenesis. Nevertheless, the precise etiology of inflammaging and its potential causal role in contributing to adverse health outcomes remain largely unknown.”
- Hand LE, Hopwood TW, Dickson SH, et al. The circadian clock regulates inflammatory arthritis. FASEB J. 2016 Aug. PubMed 27488122 ❐ This research describes a protein, cryptochrome, used by the body’s “biological clock” to repress inflammation during the night, strongly suggesting that inflammation probably varies in a daily rhythm controlled by the brain. “The clinical implications are far-reaching,” said Thoru Pederson, Ph.D., Editor-in-Chief of The FASEB Journal.
- Wright LJ, Schur E, Noonan C, et al. Chronic pain, overweight, and obesity: findings from a community-based twin registry. J Pain. 2010 Jul;11(7):628–35. PubMed 20338816 ❐
Does it hurt to be heavy? It seems possible, and in this study “obese twins were more likely to report low back pain.” But it’s not that simple: there are many variables involved. For instance, several other pain problems were also more likely: “migraine headaches, fibromyalgia, abdominal pain, and chronic widespread pain.” Weight is associated with more pain in general, not low back pain specifically, as you’d expect if the problem were simply due to compression of the spine. Clearly that typical assumption is not a safe one, and indeed the apparent connection between weight and pain weakened when the data were adjusted for common denominators like depression, a strongly confirmed risk factor for low back pain. In other words, if you factored out the depressed cases, the remaining subjects were not all that likely to have back pain. Given such complexity, the researchers made it clear that more and different research is needed to figure out what, exactly, is causing what. No kidding!
- Mäntyselkä P, Kautiainen H, Vanhala M. Prevalence of neck pain in subjects with metabolic syndrome—a cross-sectional population-based study. BMC Musculoskelet Disord. 2010;11:171. PubMed 20670458 ❐ PainSci Bibliography 53456 ❐ This study found that neck pain is prevalent in people with metabolic syndrome. The relationship is definitely not necessarily causal, but it certainly might be. This evidence certainly suggests a need for more research to find out.
- Stubbs B, Vancampfort D, Thompson T, et al. Pain and severe sleep disturbance in the general population: Primary data and meta-analysis from 240,820 people across 45 low- and middle-income countries. Gen Hosp Psychiatry. 2018 May;53:52–58. PubMed 29807277 ❐
This study dove into data on both pain and severe sleep problems around the world, finding that they are “highly co-morbid.” That is, they go together: people who have sleep problems have pain, and people with pain have sleep problems. Duh? No one is going to be shocked by that, but this conclusion did not come from the usual suspects.
Science tends to focus on “subjects of convenience.” For instance, psychology studies are notorious for recruiting their subjects from the hungry university students they’re surrounded by: “Free pizza if you put up with a bit of zapping!”
But uni students are like a sub-species of human, and so what we “learn” about psychology from them is often not true of anyone else — a great example of why we take studies with a grain of salt.
Science also tends to focus on data of convenience, and so there was “a paucity of multinational population data” about pain and sleep deprivation. Stubbs et al. set out to fix that by using a lot of data from low- and middle-income countries, about almost a quarter million people — how’s that for a good sample size? And they found the same link that has been seen many times before in the more convenient and plentiful data from the richest countries, confirming that the link exists everywhere. And that what was not actually a given, however obvious it might seem.
There is a potent chemistry between sleep and health, and it is definitely not just a case of the “worried well” sweating the little stuff in our relatively comfortable lives. This data strongly suggests that the sleep-health link matters no matter who you are or where you’re from — it’s a basic feature of being human.
- Gerhart JI, Burns JW, Post KM, et al. Relationships Between Sleep Quality and Pain-Related Factors for People with Chronic Low Back Pain: Tests of Reciprocal and Time of Day Effects. Ann Behav Med. 2017 Jun;51(3):365–375. PubMed 27844327 ❐ PainSci Bibliography 51845 ❐
- Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci. 2012 Jul;1261:88–96. PubMed 22823398 ❐
The most pertinent passage from this wide-ranging review:
In addition to the well-documented consequences of low-grade inflammation on the cardiovascular system, for example, the literature summarized here further shows that stress-induced IL-6 increases are closely linked to fatigue and reduced sleep quality. Since sleep is important also for recovery from psychological stress, long-term or repeated stress-induced activation of inflammation is a maladaptive response.
For inflammatory conditions in particular, these findings add important insights to the well-understood effects of anemia and nighttime pain through inflammation, which is also mediated by IL-6. Evidence clearly suggests that changes in circulating IL-6 can cause changes in sleep quality. Conversely, reductions in sleep duration, quality, or efficiency are capable of increasing peripheral IL-6 concentrations. These results are probably related to the fact that IL-6 increase can also be observed in chronic stress, as a consequence of long-term changes in stress system activity. Taken together, these findings, from various fields of research, underscore the close relationship between IL-6 signaling with CNS processes, thereby making IL-6 a promising candidate for linking adverse CNS states with physical disease.
- Manson JE, Patsy M B, Rosen CJ, Taylor CL. Vitamin D Deficiency — Is There Really a Pandemic? N Engl J Med. 2016 Nov 10;375(19):1817–1820. PubMed 27959647 ❐
ABSTRACT
The claim that large proportions of North American and other populations are deficient in vitamin D is based on misinterpretation and misapplication of the Institute of Medicine reference values for nutrients — misunderstandings that can adversely affect patient care.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008 Apr;87(4):1080S–6S. PubMed 18400738 ❐ PainSci Bibliography 55028 ❐
- Steffens 2015, op. cit.
- There is a distinction between “discomfort” and having significant back pain. Sitting a lot at work is not linked to back pain (see Lis, Bakker, Chen). The discomfort we feel when we sit too still for too long time does not seem to be a risk factor for serious episodes of back pain.
- There’s no direct evidence for this. It’s a claim that has often been made by clinicians and experts on the topic. Although no one knows exactly what makes trigger points flare up (or go away), extremes of activity and stimulation — too much and too little — are plausible possibilities that seem to be consistent with what patients often report.
- I ripped up my shoulder joint playing ultimate (a Frisbee sport). It was hard to sleep for most of a year. When I did sleep, I routinely rolled onto the injured shoulder. Sometimes it woke me up; if it didn’t, I’d wake up with my shoulder howling. And then it would calm down and be mostly fine for the rest of the day. I knew exactly why I had morning shoulder pain, but what if my shoulder was vulnerable for some less obvious reason? I might have thought I had unexplained “morning shoulder pain.”
- Desouzart G, Matos R, Melo F, Filgueiras E. Effects of sleeping position on back pain in physically active seniors: A controlled pilot study. Work. 2015;53(2):235–40. PubMed 26835867 ❐
- Tetley M. Instinctive sleeping and resting postures: an anthropological and zoological approach to treatment of low back and joint pain. BMJtetley00. 2000;321(7276):1616–8. PubMed 11124203 ❐ PainSci Bibliography 53595 ❐
Could “paleo sleeping” help aches and pains? This short, bizarre old paper in the British Medical Journal offers some interesting raw data about “instinctive” sleeping postures in primates. Unfortunately, the author’s interpretation is so grandiose and silly that I have to mostly just roll my eyes at it. From the introduction:
You probably do not know that nature has provided an automatic manipulator to correct most spinal and peripheral joint lesions in primates. In common with millions of other so called civilised people you suffer unnecessarily from musculoskeletal problems and are discouraged about how to treat the exponential rise in low back pain throughout the developed world.
That’s mighty big talk! All you have to do is sleep on the ground, and all your body pain will be solved! Sheesh.
The whole thing is a classic example of wishful thinking based on romanticizing “primitive” and “natural” lifestyles. Specifically, I think the premise that primitive people have fewer musculoskeletal complaints at all — let alone that it’s due to sleeping postures — is undoubtedly the product of confirmation bias and not remotely reliable. It could be true, but it probably isn’t. It’s much more likely that it’s just what western observers see because it’s what they want to believe. The extremely poor reasoning on display in this article does no favours to the hypothesis.
And, oh dear, there are way too many references for “correcting” joints! What does that even mean? The absurdity peaked for me with this statement:
The Achilles tendon of the leading foot can be inserted in the gap between the big toe and the first lesser toe to help correct a bunion.
What utter bollocks! This is the hubris of structuralism at its worst.
- A few years ago, I got keen on trying to figure out “once and for all” what kind of sheets I really like. I bought several sets of sheets of different kinds and qualities, including some expensive ones. Despite the expense and the effort, the experiment was a failure: I wasn’t organized enough, and simply couldn’t keep track of the relatively subtle differences between sheets. But I did at least learn that I have no obvious preference for premium sheets. 😉
- Jacobson BH, Boolani A, Dunklee G, Shepardson A, Acharya H. Effect of prescribed sleep surfaces on back pain and sleep quality in patients diagnosed with low back and shoulder pain. Appl Ergon. 2010 Dec;42(1):91–7. PubMed 20579971 ❐
We often worry about lying awake in the middle of the night — but it could be good for you. A growing body of evidence from both science and history suggests that the eight-hour sleep may be unnatural.
Indeed, all the research indicates that humans aren’t actually built to sleep through the night (with the exception of my wife, apparently, who can sleep 10 hours without so much as rolling over). The wakeful patch tends to occur between about 2–4. I discuss this more in my insomnia tutorial.
- Matsumura Y, Kasai Y, Obata H, et al. Changes in water content of intervertebral discs and paravertebral muscles before and after bed rest. J Orthop Sci. 2009 Jan;14(1):45–50. PubMed 19214687 ❐
- Belavý DL, Miokovic T, Armbrecht G, Felsenberg D. Hypertrophy in the cervical muscles and thoracic discs in bed rest? J Appl Physiol (1985). 2013 Sep;115(5):586–96. PubMed 23813530 ❐
- Belavy DL, Adams M, Brisby H, et al. Disc herniations in astronauts: What causes them, and what does it tell us about herniation on earth? Eur Spine J. 2016 Jan;25(1):144–54. PubMed 25893331 ❐ “The most likely cause for lumbar IVD herniations was concluded to be swelling of the IVD in the unloaded condition during spaceflight.”
- Annular tears or basically arthritic fissures in the disc — splitting like chapped lips. “Annular” because the lesion is in the annulus fibrosis, or outer layer of the disc.
