Neuropathies Are Overdiagnosed
Our cultural fear of neuropathy, and a story about nerve pain that wasn’t
This was a full-page advertisement for Lyrica in National Geographic magazine back in the 2000s:
“Do you feel burning pain in your feet?” the ad asks. “Or uncomfortable tingling, numbness, stabbing, or shooting sensations? If so, you may have nerve pain.”
Yes, you might. But it’s not actually all that likely. Neuropathy is pain caused by trouble with nerves themselves, rather than something they are detecting, and one of the three major kinds of pain. Neuropathy is probably a lot less common than most people believe.1 Many other common causes of pain and altered sensation routinely fool patients and professionals alike into suspecting “some kind of nerve problem.”
This article discusses our cultural fixation on nerve pain, the basics of neuropathy, the misuse of drugs like Lyrica, the extraordinary wiggle room that spinal nerve roots have, and tells the story of a young woman who only seemed to have a roaring case of sciatica.
Nerves are notorious
Nerves make people nervous! The whole idea of nerves gets people anxious. Could it be a nerve? People are likely to wonder if any puzzling pain. Is this a nerve problem? What if it’s a nerve? Is something pinching my nerve? Something must be pinching a nerve!
The ad with the stinging ants is a great example of advertising that inflames anxiety about nerves. Pfizer and other pharmaceutical companies spent about a kajillion dollars on marketing that can create more worry about nerve pain in a year than I can counteract in an entire lifetime of low-budget public education! Bummer.
What is neuropathy?
Neuropathy is symptoms caused by interference with normal nerve function. The symptoms of neuropathy include:
- pain, especially “zapping” and “burning” pains, and not so much “aching”
- weird sensations (especially tingling), collectively known as parasthesia (altered sensation)
- numbness
- weakness
Most neuropathy is peripheral neuropathy: trouble with a nerve that is distant from the spinal cord, like Baxter’s neuritis in the foot, or carpal tunnel syndrome in the wrist, usually causing quite specific symptoms. The big nerves emerging from the spine — the nerve “roots”, or their major branches — are the next major category, radiculopathy, which often causes more complex and widespread symptoms. Sciatica is known for being a bit of both, but most neuropathies fit well into one category or the other, or the extremely diverse “central” neuropathies of the spinal cord and brain.
Adding insult to injury: anticonvulsants for neuropathy are perfidious
Anticonvulsants like Lyrica and Neurontin (the “gabapentinoids”, mostly pregabalin and gabapentin) are badly abused — an important way to make the case that neuropathy itself is also overdiagnosed.
These drugs were originally for epilepsy … which was expanded to neuropathic pain (with some justification) … but then their off-label use for other conditions was aggressively and illegally promoted until they were among the most over-prescribed and abused pharmaceuticals in history. They are only partially effective for epilepsy and neuropathy, and hardly at all for much of anything else.
But they are addictive sedatives that make people so dizzy and woozy that they have caused a huge surge in hip fractures (and very likely many other kinds of accidents).2
Much of the modest efficacy they seem to have is may just be the sedation talking. (It’s easy to mistake sedation for analgesia.)
These drugs are magic bullets for neuropathy. The original big leap of logic was that a drug that could ease epilepsy might also tame other kinds of nerve dysfunction — which is only partially true.34
And they are definitely not effective for back pain and sciatica5 — still one of the most common reasons for their use in 2025 (maybe the most), despite clear guidelines to the contrary for several years now.6 And why would anyone have thought they were good for back pain in the first place? That makes almost no sense at all … until you follow the money to one of the biggest scandals in modern medicine.7 The illegal marketing of these drugs for off-label uses is one of the most notorious examples of Big Pharma living up to its reputation for evil-doing … but of course it’s far from the only example of fear-mongering to sell unproven uses for drugs.8 It’s just the worst.
More anticonvulsants, more!
Thanks to that horror show, and to research by Peet et al., we now know there was a mighty 5× surge in gabapentin prescribing in the 2000s and 2010s,9 despite the dubious value for most of what it was being prescribed for (most kinds of pain).
They work for seizures, why not back pain? Hmm, might want to test that idea before selling it. Anticonvulsants never really made a lick of sense for many kinds of pain, especially back pain — but the claim was sure profitable.
Interestingly, those prescriptions weren’t replacing opioids. The anticonvulsants scandal did nothing but complicate the opioid crisis, because the immense increase in their prescription was more with opioids than instead of them: overlapping prescriptions tripled. Why? Why?! That’s just bonkers. But there is a tragic logic to it. Journal Watch in early 2023:
“Clinicians clearly are turning to gabapentin as a nonopioid option for pain management or adding it to opioid treatment to avoid escalating opioid doses. Clinicians should not view gabapentin as a panacea for chronic pain management and should be especially wary of coprescribing it with opioids.”
So: doctors are collectively trying to mitigate the opioid crisis by prescribing drugs that don’t work for most pain, mainly because they was aggressively promoted. •slow clap•
This does not remotely mean that all medicine is corrupt or useless, or even that all prescriptions for anticonvulsants are bogus; these drugs have legitimate uses. But their abuse is a dark stain.10
What could demonstrate the overdiagnosis of “nerve pain” better than the overwhelming evidence of over-prescription of the gabapentinoids?
Nerve roots actually have a lot of wiggle room
The idea of a pinched nerve root particularly is deeply embedded in the public consciousness. But…
It’s difficult to actually pinch most nerves, or nerve roots (as they exit the spine). Most nerves have generous “wiggle room.” In the lumbar spine, the holes between the vertebrae that nerve roots pass through can be more than a couple centimetres at their widest, while the nerve roots themselves are only about 3-4mm thick.11 If you stretch or compress the spine, the holes do change size a little — as much as 70–130% in the looser neck joints,12 a little less in the low back.13 But, even at their most compressed, there’s still plenty of room.
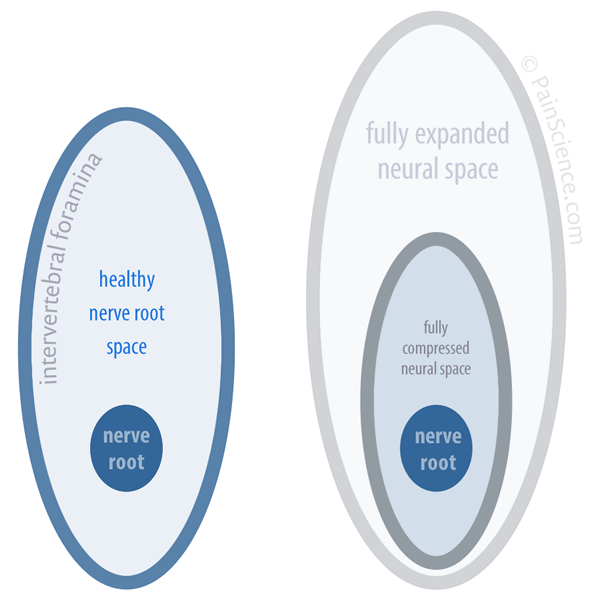
Schematic of nerve root wiggle room
On the left are the approximate proportions of a healthy nerve root and the hole it passes through (intervertebral foramen). When the spine is pulled or compressed, the holes get a little larger or smaller, as shown on the right … but there’s still lots of nerve root room.
There’s so much space for nerve roots that significant arthritic deformation and even major derangements of the spine (dislocations, spinal stenosis) can fail to actually cause trouble.1415
A young woman story about nerve pain that wasn’t really nerve pain
I once helped with a young woman who had “sciatica” — the mother of all nerve pinches. The sciatic nerve is the biggest single peripheral nerve in the human body. Allegedly, either her sciatic nerve, or one of the lumbar nerve roots it emerges from, was being pinched and sending hot zaps of pain down her leg.
That can happen, so it was a plausible diagnosis, and she came to me with it already accepted. She also had some tingling in her feet. Her symptoms did indeed sound a lot like a nerve impingement problem. On the face of it, it was likely that her sciatic nerve was irritated: true sciatica, a genuine neuropathy.
A couple things didn’t add up, though. For instance, she had no numbness at all — no dead patches of skin, which are highly characteristic of true nerve impingement. Instead, she had widespread “dead heaviness” in her leg, a different kind of numb feeling that is much more closely associated with “muscle knots” than nerve pinches — and a lot more common.
I quizzed her carefully about the quality of her pain. She assured me it was “zappy” and “electrical” … just as you would expect of nerve pain, not knots. Yet something didn’t seem quite right. I couldn’t shake the impression that she was interpreting non-neurological pain as an electrical mainly due to her strong belief that she had a nerve problem. When you think a pain is nervy, you’re going to interpret, feel and describe it in nervy terms. Pain quality is an extremely flexible concept.
So I did some experimenting, and clinched the case:
This young woman’s “nerve” pain could be perfectly mimicked (provoked) by gentle prodding of muscle tissue that was nowhere close to the sciatic nerve or it’s alleged entrapment by the piriformis muscle. Pressing on the side of her hip, on the gluteus medius muscle, several centimetres away from the sciatic nerve, she reported the same “electrical” pain flowing down her leg. It even stimulated the weird, tingling sensations in her foot.
That largely eliminated a diagnosis of sciatic nerve impingement, and the symptoms were fairly easy to relieve. No more neuropathy.
A more likely story
In spite of spending most of my career trying to explain to people that pain has many possible causes, and that muscle pain is particularly common and sneaky, I was surprising myself — fooled, really.
I suspect that muscle knots are routinely doing this, fooling patients and professionals alike. Painful trigger points are definitely more common than neuropathy, and at least some of those muscle knots feel enough like nerve pain that they are easily mistaken for the more familiar bogeyman.
Do you feel burning pain in your feet? Or uncomfortable tingling, numbness, stabbing, or shooting sensations? If so, you are more likely to have muscle pain than nerve pain — or something else entirely. Nerve pain is only one of many possible explanations for such symptoms (see 38 Surprising Causes of Pain). But muscle pain is one of the most common and reassuring, and it’s safe and easy to experiment with.
I have written three books on related topics. For more information about muscle knots, see the free introduction to The Complete Guide to Trigger Points & Myofascial Pain I also explore nerve pain overdiagnosis in detail in my neck pain and low back pain books. Some other sub-topics about our fear of nerve pain that they cover in more detail:
- detailed comparison of nerve and muscle pain
- more colour about our cultural fear of neuropathy (meet the Italian “it’s-a-nerve-eh?” guy!)
- more about how the “sciatica” might be explained and how trigger point pain and neuropathy can be similar
- more about how treatment of muscle pain may help neuropathy
- much more about how muscle pain might, ironically, be a poorly understood kind of neuropathy
- an explanation of how pinching in itself is not enough to cause neuropathy (seriously), and some dramatic examples of painless nerve impingements
The Complete Guide to Trigger Points & Myofascial Pain
Myofascial trigger points — so-called “muscle knots” — are increasingly recognized as a factor in many of the world’s aches and pains. This book-length tutorial focuses on advanced troubleshooting for patients who have failed to get relief from basic tactics, but it’s also ideal for starting beginners on the right foot, and for pros who want to stay current and as science-based as possible. 184 sections inspired by the famous texts of Drs. Travell & Simons, but also much more recent science. Buy it now for $19.95 or read the first few sections for free!
Paying in your own (non-USD) currency is always cheaper! My prices are set slightly lower than current exchange rates, but most cards charge extra for conversion.
Example: as a Canadian, if I pay $19.95 USD, my credit card converts it at a high rate and charges me $26.58 CAD. But if I select Canadian dollars here, I pay only $24.95 CAD.
Why so different? If you pay in United States dollars (USD), your credit card will convert the USD price to your card’s native currency, but the card companies often charge too much for conversion — it’s a way for them to make a little extra money, of course. So I offer my customers prices converted at slightly better than the current rate.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
More articles about back pain, spines, and nerves …
- Don’t Worry About Lifting Technique — The importance of “lift with your legs, not your back” to prevent back pain and injury has been exaggerated
- Chronic Low Back Pain Is Not So Chronic — The prognosis for chronic low back pain is better than you think
- The Mind Game in Low Back Pain — How back pain is powered by fear and loathing, and greatly helped by rational confidence
- The Tyranny of Yoga and Meditation — Do you really need to try them? How much do they matter for recovery from conditions like low back pain?
- Spinal Subluxation — Can your spine be out of alignment? Chiropractic’s big idea has been misleading patients for more than a century
- Does Spinal Manipulation Work? — Spinal manipulation, adjustment, and popping of the spinal joints and the subluxation theory of disease, back pain and neck pain
- Organ Health Does Not Depend on Spinal Nerves! — One of the key selling points for chiropractic care is the anatomically impossible premise that your spinal nerve roots are important to your general health
- The Complete Guide to Neck Pain & Cricks — An extremely detailed guide to chronic neck pain and the disturbing sensation of a “crick”
- The Chiropractic Controversies — An introduction to chiropractic controversies like aggressive billing, treating kids, and neck manipulation risks
What’s new in this article?
Five updates have been logged for this article since publication (2007). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more
Like good footnotes, update logging sets PainScience.com apart from most other health websites and blogs. It’s fine print, but important fine print, in the same spirit of transparency as the editing history available for Wikipedia pages.
I log any change to articles that might be of interest to a keen reader. Complete update logging started in 2016. Prior to that, I only logged major updates for the most popular and controversial articles.
See the What’s New? page for updates to all recent site updates.
Apr 10, 2025 — Significant upgrades to the summary of anticonvulsants: “Adding insult to injury: anticonvulsants for neuropathy are perfidious.”
2024 — More and better detail on the over-prescription of anticonvulsants.
2023 — Science update with some substance, a bit more than just a citation: Peet et al. really adds to the case that the fraudulent marketing of anticonvulsants was a pain care catastrophe, resulting in extreme over-prescription.
2021 — Correction. I excessively demonized gabepentin and pregabalin based on an oversimplification of their legal history and inadequate attention to the evidence on efficacy for neuropathy. In fact, these drugs are efficacious for some neuropathies.
2021 — Modernized, expanded. Most importantly, I added some more basic useful information and citations about neuropathy and muscle pain. This page is still technically just an abridged excerpt, but it now stands a little taller on its own. Some improvements also transplanted back into the tutorials this page came from.
2007 — Publication.
Notes
- Braddom RL, Spitz L, Rivner MH. Frequency of radiculopathies in motor vehicle accidents. Muscle & Nerve. 2009 Apr;39(4):545–7. PubMed 19260059 ❐
This fascinating study of almost 25,000 patients showed that “pinched nerves” (nerve root impingement, radiculopathy) are fairly rare — only 6% actually had it in the neck, and only 12% in the low back — and it’s barely any more common in people who’ve had car accidents. You would think that car accidents would cause more nerve root injuries, especially in the neck, but that is precisely what this study did not find. It identified only a small (2%) increase in the neck, and no difference at all in the low back. That’s a counter-intuitive finding. If you polled health professionals and patients and asked them “Do people who’ve had car accidents have more nerve injury?” I think you would get a much larger number.
So I get two interesting things out of this straightforward study: first, it’s (yet another) great example of how the spine is not particularly fragile or prone to nerve injury; second, it’s good evidence that nerve root pinches are rare overall, certainly relatively to what people fear. Yes, 12% is more than 1 in 10 people — hardly rare — but if you believe every patient who says “I have a pinched nerve,” the rate would be about 80%!
- Leung MTY, Turner JP, Marquina C, et al. Gabapentinoids and Risk of Hip Fracture. JAMA Netw Open. 2024;7(11):e2444488. PubMed 39535796 ❐ PainSci Bibliography 50057 ❐
Leung et al. looked at data on about twenty-eight thousand older Australians with hip fractures between 2013 and 2018, whittling that down to 2600 who had consumed at least one prescription for a gabapentinoid (mostly pregabalin), and another thirteen thousand that didn’t as controls. They also studied two other major known risks for hip fracture, kidney disease (30% of the subjects) and general frailty (45%).
The main finding was that gabapentinoids are quite powerfully linked to a risk of hip fracture, via the mechanism of dizziness causing a risk of falling:
- 30% more breaks even in the healthiest subjects (1.3×)
- 75% more in the frail (1.75×)
- 140% with kidney disease! (2.4×)
Those are shocking numbers. That’s a lot of serious harm for a class of drugs that is notoriously over-prescribed for many types of pain that they mostly cannot help. I discuss this in much more detail in a blog post.
This experiment had a lot of self-control. That is, subjects acted as their own controls in multiple ways: a fancy “case-case-time-control” design that compared subjects to themselves at different times (“case-crossover”), but also to other patients across time (“case-time-control”). It’s too nerdy a design even for the salamander to ramble on about! It was fancy and interesting, and that’s enough said here (but try your luck with a good technical description).
That design means that the results probably weren’t a statistical illusion. But there were some limitations (as always): reliance on prescription data rather than actual drug use, and frailty assessments based on hospital data rather than direct clinical evaluation.
- Wiffen PJ, Derry S, Bell RF, et al. Gabapentin for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017 06;6:CD007938. PubMed 28597471 ❐ PainSci Bibliography 52185 ❐
This The Cochrane Collaboration review concludes that some people do get good relief from gabapentin for postherpetic and diabetic neuropathy, but 50% “will not have worthwhile pain relief but may experience adverse events,” and evidence for other types of neuropathic pain is very limited.
- Derry S, Bell RF, Straube S, et al. Pregabalin for neuropathic pain in adults. Cochrane Database Syst Rev. 2019 01;1:CD007076. PubMed 30673120 ❐ PainSci Bibliography 52190 ❐
This The Cochrane Collaboration review of pregabalin (Lyrica) has a clearly positive conclusion: it appears to be efficacious for postherpetic and diabetic neuralgia, plus also “mixed or unclassified post-traumatic neuropathic pain.” However, results vary widely from one person to the next, and “many will have no benefit.” All drugs are like this to some extent, of course, but the response to anti-convulsants for neuropathy seems to be particularly varied.
- Enke O, New HA, New CH, et al. Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis. CMAJ. 2018 Jul;190(26):E786–E793. PubMed 29970367 ❐ PainSci Bibliography 53209 ❐
Evidence to date does not support the use of anticonvulsants for chronic low back pain or lumbar radicular pain. This review found mostly moderate- to high-level quality of evidence suggesting no treatment benefit for pain and disability, and high-level evidence supporting the risk of harms.
- The [NICE guidelines specifically and clearly advise doctors not to offer them sciatica](https://www.nice.org.uk/guidance/ng59/resources/low-back-pain-and-sciatica-in-over-16s-assessment-and-management-pdf-1837521693637): “there is no overall evidence of benefit and there is evidence of harm.”
- Gabapentin (Neurontin) was originally approved to treat a rare type of seizure disorder and a specific type of pain but was later aggressively advertised to patients and doctors for at least eleven unapproved medical conditions (bipolar disorder, other pain syndromes, and restless leg syndrome). The manufacturer (Pfizer) paid out billions in lawsuit settlements and record-breaking fines related to the illegal promotion of these and other drugs for uses that were not shown to be safe or effective. As much as they paid, I think it’s safe to say that they didn’t actually pay enough to undo the damage, though…
- Kesselheim AS, Mello MM, Studdert DM. Strategies and practices in off-label marketing of pharmaceuticals: a retrospective analysis of whistleblower complaints. PLoS Med. 2011 Apr;8(4):e1000431. PubMed 21483716 ❐ PainSci Bibliography 53208 ❐
- Peet ED, Dana B, Sheng FY, et al. Trends in the Concurrent Prescription of Opioids and Gabapentin in the US, 2006 to 2018. JAMA Intern Med. 2022 Nov. PubMed 36409473 ❐ PainSci Bibliography 51246 ❐
- That’s all terrible news about the state of pain medicine, but I am at least happy to show that I am not a “pharma shill” — a silly accusation, but constantly hissed at health science advocates.
- Torun F, Dolgun H, Tuna H, et al. Morphometric analysis of the roots and neural foramina of the lumbar vertebrae. Surgical Neurology. 2006 Aug;66(2):148–51; discussion 151. PubMed 16876606 ❐ This was exasperatingly hard data to find for some reason, and the paper abstract begins by saying so: “There have been few anatomic studies on the foramina and roots of the lumbar region … .” This is in a 2006 paper! Hardly ancient.
- Takasaki H, Hall T, Jull G, et al. The influence of cervical traction, compression, and spurling test on cervical intervertebral foramen size. Spine (Phila Pa 1976). 2009 Jul;34(16):1658–62. PubMed 19770608 ❐
- Sari H, Akarirmak U, Karacan I, Akman H. Computed tomographic evaluation of lumbar spinal structures during traction. Physiother Theory Pract. 2005;21(1):3–11. PubMed 16385939 ❐
- Ebraheim NA, Liu J, Ramineni SK, et al. Morphological changes in the cervical intervertebral foramen dimensions with unilateral facet joint dislocation. Injury. 2009 Nov;40(11):1157–60. PubMed 19486975 ❐
Researchers dislocated neck joints in corpses to measure the effect on the size of the intervertebral foramina. (Interesting chore!) Dislocation made the spaces quite a bit larger, indicating that any nerve root pain associated with these injuries “is probably due to distraction rather than due to direct nerve root compression.”
- Andrade NS, Ashton CM, Wray NP, Brown C, Bartanusz V. Systematic review of observational studies reveals no association between low back pain and lumbar spondylolysis with or without isthmic spondylolisthesis. Eur Spine J. 2015 Jun;24(6):1289–95. PubMed 25833204 ❐
It is widely believed that spondylolysis (SL) and/or isthmic spondylolisthesis (IS) cause low back pain. If so, individuals with these conditions should be more prone to back pain (duh). This paper reviewed other studies looking for that association. They found 15 adequate studies. None of them detected an association between SL/IS and LBP. The authors speculate that the two apparent benefits of treatments may just be “due to benign natural history and nonspecific treatment effects.” They suggest that “traditional surgical practice … should be reconsidered.”