The Art of Rest
The finer points of resting strategy when recovering from injury and chronic pain (hint: it’s a bit trickier than you might think)

Bourne concentrated on rest and mobility. From somewhere in his forgotten past he understood that recovery depended upon both and he applied rigid discipline to both.
The Bourne Identity, by Robert Ludlum, p. 137
Resting “properly” is trickier and more important than most people realize. When you are injured — especially a repetitive strain injury (RSI) — how much rest is enough rest? Is there such a thing as too much rest? What if you get out of shape or lose muscle? Is it necessary to rest completely, or is it adequate to rest only the injured part? Is “taking it easy” enough, and for how long? How do you know when to lay off and when to “use it or lose it”? How can you rest anatomy that you need to use all day, every day?
These questions aren’t especially difficult to answer with regards to most ordinary injuries — you sprain an ankle, you stay off it for a while, take it easy for many weeks, slowly get back to normal … no big deal. No “art” needed there!
They become more of a challenge when there is more at stake, when you have an injury that is not healing well and is dragging on and on, or a pain problem that cannot quite be diagnosed. It is more difficult and more important when you are hurt in a way that keeps you from earning a living, or in a body part that is hard to stop using (feet), or when the amount of rest required for healing seems to be cruel and unusual punishment, as with many overuse injuries — injuries that almost always strike at the heart of your work or play.
Both patients and professionals often pay lip service to the importance of rest, while in practice are nearly ignoring it, or even defying it. Patients are often even encouraged to do precisely the opposite of rest: to “work through” their pain, to push too hard too soon, to value on-going performance and fitness over rehabilitation. The number of cases where resting is actually treated like a meaningful strategy seem to be outnumbered about 10 to 1 by the cases where it is given only the most token consideration.
Until those numbers reverse, it’s a topic well worth writing about.
The most common objection to resting: the fear of getting out of shape
People tend to think rehab is all about a gruelling regimen of therapeutic exercise. That’s the cliché — lots of movie montages have shown it that way. But that’s rarely how it happens. It’s usually lazier.
Before we get rolling, I want to quickly shoot down the most common objection to the suggestion to rest thoroughly: the fear of “going to pot” or getting critically out of shape. This fear is often expressed by the most fit people, who are actually in the least danger. They also often tell me that they have been “warned” by their doctor (or therapist) that staying in shape is more important than resting, and that they need to be “careful” not to rest too much. That’s backwards! In general, rehabilitation should almost always put physical conditioning on the back burner, especially at first. Worry about healing first, and then concern yourself with restoring any fitness you have lost. Why?
- You certainly will go to pot if you never heal. Long-term pain is a much greater threat to your fitness than short-term resting. And nothing will keep an overuse injury going like more use!
- Peak conditioning is vulnerable, but the bulk of your fitness is actually quite stable and hard to lose. No one goes completely to pot in 3 months. Or even six. And even if you do get out shape, it’s really not that big a deal to get back into shape.
- It’s also usually easy to rest/protect an injury while still maintaining some fitness by exercising in other ways (known as “relative rest”).
- If you’re specifically worried about gaining weight, there are many experts saying loud and clear that calorie intake is by far more relevant to fatness than exercise. Do your best to eat less when you’re not exercising (and of course that’s not necessarily easy).1
Keep perspective: even people with extremely serious injuries, far worse than any case of runner’s knee or shin splints, eventually recover their fitness.2
First things first: you have to be healed before you can maintain or develop fitness, let alone optimize it.
Obviously, if you don’t exercise at all, it is not good for you. Exercise improves your health. And a lot of exercise improves your health a lot. But that doesn’t mean that insanely large amounts of exercise are insanely good for your body. At some point, too much begins to damage various physiological systems. Everything in physiology follows the rule that too much can be as bad as too little. There are optimal points of allostatic balance.
Why Zebras Don’t Get Ulcers, by Robert M Sapolsky, 123
“Bed rest” is dead
Let’s get this out of the way early as well: bed rest (a.k.a. total rest) is pretty much dead as a concept in rehabilitation. These days, doctors won’t even cast a fracture if they can avoid it — fractures heal faster when they aren’t completely immobilized.3 Even a hip fracture doesn’t get you a get-out-of-exercise card any more.4
Replacing bed rest is the concept of “early mobilization” or “active rehabilitation.” The idea is to get you moving as soon as possible — short of actually reinjuring you.5 A great deal of scientific evidence suggests that the stimulation of movement, especially in the early stages of healing, is a crucial part of recovery from injuries and surgeries.
Acute low back pain has been shown to respond much better to normal activity than to bed rest.67 Achilles tendon ruptures have been shown to heal faster with early mobilization after surgery.8 Whiplash victims recover much faster if they get moving right away after their accident, rather than wearing a collar.9
All of this is why therapeutic exercises like PF-ROM, mobilizations, functional training, reflex stimulation, endurance training, and many more are such a crucial part of serious rehabilitation.
On the other hand, sometimes active rehabilitation is too active …
You can’t exercise your way out of every problem
There is a common attitude in rehabilitation circles that patients can exercise their way out of any problem. Patients are routinely encouraged by health professionals at every turn to challenge their tissues with therapeutic exercise. They receive this advice despite a strong possibility that continued exercise is exactly the wrong thing to do, especially early in rehab.
Long before breaking under a strain, tissue often gets “sick” — a failure to keep up with maintenance and repair to match the strain. Once that happens, the tissue loses the ability to tolerate even minor stresses. Activities that used to be just fine are suddenly a problem. There’s only one way out of that trap: adequate rest is critical. You have to almost completely stop challenging the tissue, or it will never have a chance to recover.
I have seen countless examples over the years of people that I believe have suffered years of chronic pain simply because they never rested adequately. (They may think that they have, but “taking it easy” for a couple weeks is often not actually enough rest.) This predicament is particularly tragic because rest is so cheap and safe that there’s hardly any reason not to try it.
And yet patients are often pushed to exercise too hard, too soon. Why? A little history …
In 1995, a publicly owned insurance company published a report about whiplash, authored by an organization called The Quebec Task Force on Whiplash-Associated Disorders.10 People in my line of work refer to this report as “The Quebec Task Force,” or even just “Quebec” as in “In 1995, Quebec recommended active rehabilitation,” as though the province of Quebec was somehow personally involved.
“Quebec” was bullish on the whole idea of active rehabilitation, and more or less gave insurance companies everywhere a great reason to push people hard through rehabilitation. Countless insurance adjusters, physiotherapists and doctors started telling accident victims to get back into the gym as soon as possible. But how do you define “as soon as possible”?
Unfortunately, many fans of the QTF were pretty aggressive about it. I’ve seen cases where people were sent to the gym to do strength training exercises within days after an accident, when the tissue is still inflamed. Those of us less enthusiastic about the QTF11 witnessed a huge increase in the number of patients who had been pushed much too hard, much too soon. Yikes.
There is a balance to be struck. On the one hand, it’s clear that early mobilization and general activity is valuable. On the other hand, it’s just as clear that you can aggravate and even re-injure yourself by trying to do too much, too soon. If you feel that a physiotherapist or doctor is pushing you too hard, there’s a good chance that they are.
Re-injury and collateral injury12 are real risks. People get hurt trying to get over being hurt all the time. Keep this in mind!
Patellofemoral pain: the perfect example
Of all the repetitive strain injuries, patellofemoral pain is probably the trickiest to rest effectively. Patellofemoral pain is a type of runner’s knee that affects the joint between the femur and kneecap. It’s unusually sensitive to over and underloading, and can take a long time to recover even under optimal conditions, and so it’s more difficult and more important to rest PFPS properly than other conditions. It emphasizes everything about the challenge of resting.
It’s tricky because the patellofemoral joint is naturally a high performance joint that tolerates intense pressures under the kneecap … even when you aren’t doing anything impressive with it. And when you make a point of exercising your knees, the intensity goes up way more than most people realize. And so, unlike most other RSIs, you can easily overuse your patellofemoral joint without even realizing it.
For most RSIs, getting the rest right is still an interesting challenge. For patellofemoral pain, it’s more like driving a sports car with super sensitive steering. Writing a book about patellofemoral pain forced me to think quite deeply about what it meant to “rest properly.”
Is there any science about how well resting works, or the best way to do it?
Not really, no. We have no evidence-based guidance on how much resting is effective, or exactly what tactics work best. The importance of resting seems to be too obvious for science to bother testing directly.
We really know nothing about exercise dosage for any kind of chronic pain, and exercise dosage is just a mirror image of resting dosage: less exercise is the same as more resting.13
One of the main conclusions of a major review of “How much is too much?” is that there’s not enough research, and what we do know is mostly from limited data about a few specific sports.14
I really wish someone would do a nice controlled test comparing “extreme” resting for runner’s knee (avoiding most knee stress from any source) to ordinary resting (avoiding obvious sources of knee stress from running or workouts, but otherwise carrying on as normal).
But that’s a pipe dream. I doubt I will see it in my lifetime.
There are scraps of relevant research here and there, but mostly we have to read between the lines of research on the risks of excessive loading in sport. If too much loading, too fast, is the major risk factor for injury, that strongly suggests that less and slower loading — “resting” — is probably effective injury prevention… and what prevents ITBS often also treats it. So I am not exactly going too far out on a science limb recommending good rest.
Bottom line: my resting advice is based on scientific plausibility, relatively low-cost, and virtually no harm. But not, unfortunately, not a stitch of directly applicable research — not even close.
Relative rest and allowing adequate recovery
The art of rest is mostly the art of “relative” rest: finding a way to stay active and fit without placing stress on injured or severely fatigued tissues. Like rest in general, it is a neglected concept in rehabilitation. The challenge can and should be tackled with precision and creativity. Done right, it can be the closest thing there is to a “miracle cure” for many common repetitive strain injuries for which there is virtually no other effective treatment.
There are three kinds of people who need relative rest:
- Inactive people who suddenly lose the ability to continue doing the only exercise that they were getting before injury. For instance: a self-confessed couch potato who walks several blocks to work every day, but then stops doing even that when she gets a case of plantar fasciitis.
- Determined, frustrated athletes who find it “impossible” to stop running, or cycling, or swimming, or playing soccer, or whatever it may be that they are passionate about. For instance: a serious runner who gets iliotibial band syndrome, but continues to run 5k/day and claims to be “taking it easy.”
- Healthy, active people who want to optimize their fitness and reduce injury risks.
All of these people need to rest relatively. Even though they have different priorities, their needs overlap a lot: they all need to give some specific tissues a break for the sake of rehab, while continuing to challenge other tissues for the sake of general health and fitness. The need to avoid stressing injured tissues is obvious. It’s less obvious how the same principle applies to healthy active people — but still very important.
Surprisingly similar: recovery from injury and recovery from exercise
Every workout is like a mild injury that you have to recover from, shielding yourself temporarily from additional stress on the recovering tissues. And yet few active people and amateur athletes give their tissues enough time to recover and adapt. This can really increase the risk of injury, lead to feeling run-down, and is far from optimal for fitness.
For instance, it’s extremely common for people to go back to the gym long before their muscles have fully healed from the last workout.17 Progress may be less than it could be, and a sneaky hazard of overly frequent training is that it sucks to be perpetually not quite recovered.
You never actually get to enjoy your full fitness if you are too active, too often. Guys keen on the gym are particularly prone to this, spending far too many days of the month feeling sore and weak — strength remains reduced for days after the obvious sore phase is over — instead of actually feeling and enjoying their full power. It’s most obvious in their case, but the same thing applies to nearly any kind of intense workout: not only do you need adequate rest, you need to spend some of your time actually enjoying the fruits of your labours! How “fit” can you possibly be if you never allow yourself to recover?
Just as injured people must find ways of being active while protecting their vulnerable tissues, the healthy athlete can optimize training and prevent injury by carefully alternating between different kinds of stresses. A common, obvious example is to switch between upper body and lower body workouts — resting half the body while challenging the other half.
You can get a lot more creative than that, though. There are many relative rest tips, tricks and strategies …
Ideas for resting relatively
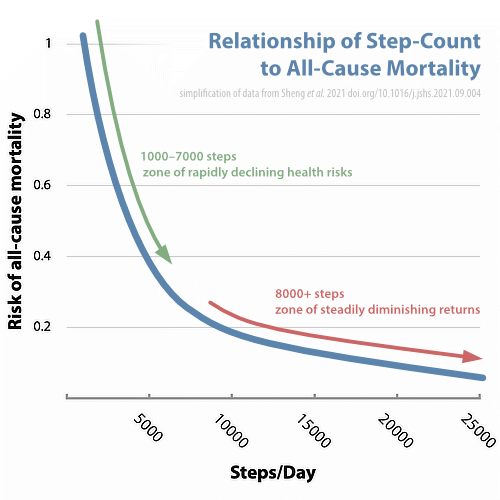
- As long as you don’t have a hip or leg injury, walking is amazingly good exercise, even at much lower doses than the notorious 10,000-steps/day goal18 — and therefore less loading.
- Swimming is one of the most classic options for relative rest. Obviously it’s not completely stressless: you’re not going to want to swim with injured shoulders at all, and the common knee injuries can be a problem. But you can really do a lot in the water with minimal risk/stress.
- Do a “thermal workout” — exhaust yourself with heating and cooling. For example, switch between a hot tub and a swimming pool. (See the thermal workout section in Contrast Hydrotherapy.)
- Being chilly is another surprisingly exhausting and almost totally passive “workout.” Turn the heat down, put on a T-shirt, and put up with being non-warm for a while.
- Vigorous breathing is a terrific non-standard workout, with numerous benefits: see The Art of Bioenergetic Breathing.
- Power yoga can certainly be intense and hard on the body, but often in a completely different way than most of your other exertions, so it can be a great way to spread the physical stress around.
- Many people who do not normally strength train in a gym should seriously consider it during rehabilitation, because it is a much better and more efficient way to stay in shape than most people realize, and the precision of gym equipment allows you to easily protect your injury while you heal.
And that was just off the top of my head.
Relative rest will come to you naturally if you like to be active, but also respect the importance of taking it easy on your injury. You will be motivated and creative in your quest for alternative activities for the duration of healing.
Warning: are you really resting?
Some patients (you know who you are) take the idea of relative rest as a sort of blank cheque to train and workout as hard as they want, as long as they aren’t directly or obviously irritating their injury. If this is you, you need to carefully ask: are you really resting?
Many activities that do not cause symptoms as quickly as others are still a problem — just less of one. Consider the following classic example:
A runner has plantar fasciitis, a kind of tendinitis19 on the sole of the foot, and running on pavement clearly irritates the condition within fifteen minutes, so he sensibly refrains from running altogether. Cycling, however, feels fine to him, and so he insists on cycling for an hour every day instead of running: relative rest, right? Maybe …
Unfortunately, cycling — especially in clips — is potentially irritating to plantar fasciitis, albeit less obviously so than running on pavement. It might take up to 90 minutes of cycling before you felt a problem, yet every hour-long ride is causing about two thirds of that irritation. This example person is not really resting at all, and will likely say things like, “I don’t understand it, I rested from running for six weeks and the problem is still just as bad as ever!”
These are the kinds of complexities that make up the art of resting!
Handling awkward body parts
Some injured locations are harder to rest than others. Take the feet, for example. (Other tricky locations are the knees, the dominant hand or wrist, the neck, and any body part essential to your job.)
Using plantar fasciitis as a good example again: it’s a painful condition, but not usually crippling. Yet every step is an irritation that keeps it going, or makes it worse. As long as you keep using your feet, it’s probably not going to go away. In such cases, people often think that they have already done enough resting, when in fact they have done no better than “taking it easy” for a few days. I’m going to pick on runners again, because they are invariably the worst offenders:
ME: Have you tried resting?
RUNNER: Yes, I really took it easy for a month.
ME: Did you stop running?
RUNNER: Stop? Oh, no, I just dropped down to 10K.
ME: A week?
RUNNER: A day.
ME: Sounds like you were still running quite a bit.
RUNNER: There was the half marathon, too …
Runners are often their own worst enemies!
But for all patients, healing from plantar fasciitis does seem to require an unfair and unreasonable amount of inconvenience: this nagging pain in your feet, a mere irritated slip of connective tissue, can require nearly as much rest as a broken leg in the worst cases.
Unfortunately, hardly anyone takes plantar fasciitis seriously enough to rest as much as they need to. A change in perspective may be necessary: think of your feet as broken, and you’re on the right track. They are broken! And they’ll probably stay broken if you don’t get off them for a while.
So, um … how long?
Let’s recap: you know that bed rest is dead and some movement of all but the most serious injuries is important … but you can’t over do it either. I’ve explained that you can use the concept of “relative rest” to rest your injured part, but otherwise remain active. And we’ve discussed how injuries in some locations are especially tricky to rest. The astute reader will have noticed that I still haven’t said how long: there is still a need to rest something, and the $64,000-question is, “How long?”
As long as it takes, of course.
With some injuries, you can tell whether or not you’re better yet, and you don’t have to guess about how long you need to rest: you just rest until you can tell that it feels better, and then add another couple weeks just to be safe. Easy!
But lots of injuries are “quiet” when you are resting. They only act up after 30 minutes of running, say. Some injuries are completely undetectable with anything less than competition intensity. Running soccer drills might be fine, but soccer itself still impossible. Skiing itself might be fine, but falling down is still a problem.
Plantar fasciitis, medial tibial stress syndrome, whiplash, carpal tunnel syndrome, iliotibial band syndrome, tennis elbow … these common problems, and many more, can feel more or less completely fine until you’ve been working/playing for a little while, and then you discover the hard way, after already irritating it, that it’s still vulnerable. How can you know how long to rest such a condition? How can you “test” it without pissing it off again?
Every case is different. In some cases you can (sort of) test it without irritating it (much). In other cases, there is no hope of this: testing will irritate the condition and potentially delay recovery.
In these cases, you must choose between two methods: the “get it over with method” and the “if at first you don’t succeed” method.
Two styles of resting
You can see why I avoided saying “how long” at first: it depends on the individual’s situation and risk tolerance. There is no “right” answer. It’s like — exactly like, actually — trying to tell someone whether they should choose safe investments, or riskier but more profitable investments: it all comes down to your personal situation and style, and how you feel
Method 1: Get it over with …
Some people prefer the “get it over with” or “overkill” method, and choose to rest a lot on the first try, to generously rest for at least 2–3 weeks more than you really think is necessary “just in case,” and not to challenge/test your injured part at all during the rest period. The benefit of this approach is that it is virtually foolproof. The disadvantage, of course, is that you may actually end up resting much more than you actually needed to.
This method is fine for people who enjoy a better-safe-than-sorry approach to life, and for people who are patient. But if you are the sort of person who can’t wait to open your Christmas presents …
Method 2: If at first you don’t succeed …
Others are so unable or unwilling to rest that they prefer the “if at first you don’t succeed” or “go for the parking spot you want”20 method, in which you try resting the minimum amount that might work. The advantage? You might succeed on the first or second try, getting away with a relatively small amount of inconvenience.
The disadvantage, of course, is that your desire for efficiency could backfire, and you could end up having to try five progressively longer rest periods, resulting in a much larger investment in rehabilitation than if you’d just rested adequately the first time. Ouch.
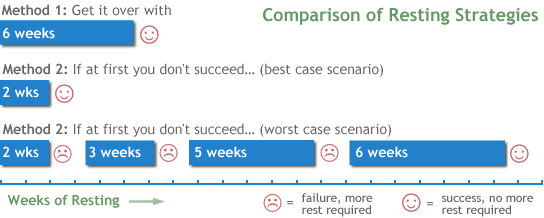
As you can see, even if you have to try twice, you might succeed on your second try and have about the same total weeks of resting as the “get it over with” method. Or you might not. The worst-case scenario with method 2 is pretty bad!
The risk is real: I once had a client, a young woman athlete with shin splints, who had tentatively tried resting for several periods of 2–4 weeks spread out over an entire year, not one of which was adequate. It was only when I counselled her to rest adequately, no matter how “painful,” that she finally started to make progress. The final rest took three full months. In all likelihood, she could have rested successfully for just 3–4 weeks on the first try, a full year before!
Here are a few more points to bear in mind when deciding how long you should try to rest:
- Old problems are usually more prone to being irritated, and usually require more rest to recover from.
- Don’t be too afraid of “testing” an injured part. There are almost always creative methods of testing that minimize stress to the injury, but can still tell you something about how it’s doing.
- It’s up to you to decide how deeply to “bury” a problem. Do you need it to mostly go away? Or completely go away? If the goal is perfection, you’re going to have to rest longer.
If you can’t take the heat …
“But I can’t do nothing!!”
“I can’t quit everything!”
“I have to do something!”
These are the howls of protest I hear from athletes and active younger people when they start to realize that “relative rest” isn’t perfect, and doing it properly means (temporarily) giving up everything they consider to be fun or rewarding. They may still be able to swim or walk or go to aerobics classes or yoga, but if they are shut out of their favourite activities — skiing, running, ultimate, whatever — they tend to think the world is coming to an end.
I sympathize. I really do! I’ve been there.21
And this is just part of being an athlete. Treat it like earning a scout badge. Rehabilitation is a rite of passage: there is hardly a serious athlete in the world who hasn’t had to go through it. Twice. Goes with the territory. If you can’t take the heat, stay out of the kitchen.
Riddle me this: which of these things is worse?
- Really truly resting for a few months, like any serious athlete has to do when they get a nasty injury?
- Never recovering at all because you just couldn’t bring yourself to rest?
Seriously, how do you think the elite athletes do it? Do you really think their coaches let them get away with abusing a badly injured piece of anatomy? Do you reckon that’s a winning strategy?
Well? Think about it! Sometimes being a “real” athlete means sucking it up and knocking it off for a while.
The hard part is just coming to emotional grips with the fact that seemingly “minor” injuries like plantar fasciitis, iliotibial band syndrome, shin splints, chronic low back pain, tennis elbow, etc, are actually not going to go away until they are actually treated like real injuries.
Enjoy your own “rehab montage.” Have fun with it. And if you can’t take the heat? Stay out of the kitchen! Give 110% to something else for a while.
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the Internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
- Pain & Injury Survival Tips — Dozens of ideas (and links) for evidence-based rehabilitation and self-treatment for common pain problems and injuries
- Sports Injury Prevention Tips — A few evidence-based ways to reduce your risk of injury
- Mobilize! — Dynamic joint mobility drills are an alternative to stretching, a way to “massage with movement”
What’s new in this article?
2021 — Science update. Added a citation to Sheng et al. about the excellent fitness bang-for-buck delivered by walking.
2019 — Added new section, “Is there any science about how well resting works, or the best way to do it?”
2007 — Publication.
Notes
- Many, many factors are involved in energy balance — not all of them under our control.
- I witnessed this firsthand in 2010, as my wife recovered from multiple fractures without any rehab heroics at all — just time and modest effort, and only after a lot of resting, when she was good and ready. She ran Vancouver’s Sun Run (a 5k) a little over a year after her car accident.
- Consider a modern example:
I had a massage therapy client in the 2000s who broke her arm and was told by her doctor: “Look, I can put this in a cast and it will be nice and safe, or we can leave it out and it will heal three weeks faster if you can protect it properly until then.” She chose to skip the cast, and was simply very careful with her arm for a little while. Sure enough, the wound was healed in excellent time. Even though she was very careful with it, the gentle stresses of gravity and slight movements alone were enough to stimulate accelerated healing.
- Oldmeadow LB, Edwards ER, Kimmel LA, et al. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg. 2006 Jul;76(7):607–611. PubMed 16813627 ❐
From the abstract: “Early mobilization after hip fracture surgery accelerates functional recovery and is associated with more discharges directly home and less to high-level care.”
- Which is not an unimportant point! Obviously there is such a thing as too much of a good thing here. For instance, in 2009, Lamb showed that severe ankle sprains heal much better when completely immobilized by a cast initially. This is a direct contradiction to the fashionable practice of aggressive active rehabilitation, in which the ankle is stabilized only by a brace or a tube bandage, and the patient is encouraged to get the joint back into the action when it’s still seriously unstable.
- Hagen KB, Jamtvedt G, Hilde G, Winnem MF. The updated cochrane review of bed rest for low back pain and sciatica. Spine. 2005 Mar;30(5):542–546. PubMed 15738787 ❐
From the abstract: “For people with acute low back pain, advice to rest in bed is less effective than advice to stay active.” There is even “high quality evidence” that bed rest leads to more pain.
- Vroomen PC, de MC Krom, Wilmink JT, Kester AD, Knottnerus JA. Lack of effectiveness of bed rest for sciatica. N Engl J Med. 1999 Feb 11;340(6):418–23. PubMed 9971865 ❐ PainSci Bibliography 56953 ❐
In this sciatica study, researchers assigned 183 subjects “either bed rest or watchful waiting” for two weeks and found that “bed rest is not a more effective therapy than watchful waiting.” Nor is it less effective. The results were exactly the same. If that sounds like no big deal, consider the difference in the lives of those patients: two weeks of bed rest, compared to two weeks of going about your business!
- Sorrenti SJ. Achilles tendon rupture: effect of early mobilization in rehabilitation after surgical repair. Foot Ankle Int. 2006 Jun;27(6):407–410. PubMed 16764795 ❐
From the abstract: “Surgery combined with early mobilization reduces range of motion loss, increases blood supply, and reduces the degree of muscle atrophy that typically occurs after Achilles tendon rupture, thereby decreasing the time to resumption of normal activities.”
- See Mealy, Vassiliou, McKinney, and Schnabel.
- Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. 1995;20(8 Suppl):1S–73S. PubMed 7604354 ❐
- Freeman MD, Croft AC, Rossignol AM. “Whiplash associated disorders: redefining whiplash and its management” by the Quebec Task Force. A critical evaluation. Spine. 1998 May 1;23(9):1043–9. PubMed 9589544 ❐
This is a strongly negative review of the well-known 1995 papers published by the Quebec Task Force on Whiplash-Associated Disorders. “Five distinct and significant categories of methodologic error were found.… Although the Task Force set out to redefine whiplash and its management … its publications instead have confused the subject further.”
- Ingraham. Sports Injury Prevention Tips: A few evidence-based ways to reduce your risk of injury. PainScience.com. 3832 words.
- Polaski AM, Phelps AL, Kostek MC, Szucs KA, Kolber BJ. Exercise-induced hypoalgesia: A meta-analysis of exercise dosing for the treatment of chronic pain. PLoS One. 2019;14(1):e0210418. PubMed 30625201 ❐ PainSci Bibliography 52661 ❐
This is a good quality review of studies of exercise for chronic pain that tried to extract some wisdom about exercise dosage for chronic pain patients. Unfortunately, it failed: the review establishes only that we know essentially nothing about exercise dosage for chronic pain patients. Our ignorance is near total. There’s just not enough of the right kind of evidence to conclude anything, and almost countless confounding factors and variables that have never been studied.
“The lack of dosing studies for exercise means that patients may not be receiving the optimal therapy and/or be receiving a therapy that actually increases pain.”
From a detailed analysis of the review:
Appropriate exercise dosage may not be generalizable beyond the individual patient given their goals and prior activity levels. … Perhaps it isn’t necessary (or even realistic) to find an optimal, generalizable dosage of exercise for pain states, but rather to find appropriate exercise dosage for the individual based on their desired goals.
- Soligard T, Schwellnus M, Alonso JM, et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016 Sep;50(17):1030–41. PubMed 27535989 ❐
- Gabbett TJ. Debunking the myths about training load, injury and performance: empirical evidence, hot topics and recommendations for practitioners. Br J Sports Med. 2018 Oct. PubMed 30366966 ❐ “Rapid increases in training and competition workloads and low chronic workloads are associated with greater injury risk. These findings suggest that appropriately staged training programmes may reduce injury risk in athletes. There is an urgent need for randomised controlled trials to test this working hypothesis.”
- How fast load can be increased without causing injury and how much rest is required without causing re-injury during rehab are not exactly the same concepts, but they are certainly very closely related. The main difference is that healthy and injured people probably have different thresholds for risk of injury versus re-injury. In short, when you’re already injured — which is the case for everyone with a stubborn overuse injury — you probably have to be more careful.
- This is covered in considerable detail in Strength Training Frequency: Less is more than enough: go to the gym less frequently but still gain strength fast enough for anyone but a bodybuilder.
- Sheng M, Yang J, Bao M, et al. The relationship between step count and all-cause mortality and cardiovascular events: A dose-response meta-analysis. J Sport Health Sci. 2021 Sep. PubMed 34547483 ❐ PainSci Bibliography 52202 ❐
This is a review and meta-analysis of sixteen studies of the relationship between step count and the risks of dying from any cause, or developing cardiovascular disease. They found a very clear connection between more walking and reduced risks, but the dose-response was strongly “non-linear.” In other words, you do not have to walk even close to 10,000 steps/day for it to be worth your while. The benefits are “non-linear”: you get a lot of benefit up front, a huge reduction in health hazards by the time you’ve hit 5K steps… at least double what you get out of the next 5K. These results challenge the popular goal of 10,000 steps per day being “optimal” for health.
![]()
This is an inexact but correct-in-spirit rendering of the most important graph in Sheng et al.
For more on this study, see: Big health benefits from far fewer than 10k steps per day.
“Tendinitis” versus “tendonitis”: Both spellings are acceptable these days, but the first is the more legitimate, while the second is just an old misspelling that has become acceptable only through popular use, which is a thing that happens in English. The word is based on the Latin “tendo” which has a genitive singular form of tendinis, and a combining form that is therefore tendin. (Source: Stedmans Electronic Medical Dictionary.)
“Tendinitis” vs “tendinopathy”: Both are acceptable labels for ticked off tendons. Tendinopathy (and tendinosis) are often used to avoid the implication of inflammation that is baked into the term tendinitis, because the condition involves no signs of gross, acute inflammation. However, recent research has shown that inflammation is actually there, it’s just not obvious. So tendinitis remains a fair label, and much more familiar to patients to boot.
- Some people assume that they aren’t going to find the best parking spot, so they don’t even try. But you’ll never get the best parking spot if you don’t check!
- In 1996, I discovered the sport of ultimate, and was instantly addicted … only to get a nasty case of iliotibial band syndrome about one year later. I didn’t know how to treat it back then, and I went through several stages of not-quite-enough-rest for two full years, because it was very hard for me to stay out of the game.