Sports Injury Prevention Tips
A few evidence-based ways to reduce your risk of injury

Sadly, medical science has yet to figure out how to clearly identify people who are at risk for sports injuries.12 Injuries happen, but we mostly don’t know why they happen to the people they happen to, so prevention is a bit of a crapshoot. This article reviews some of the closest things we have to evidence-based injury prevention options.
But first, let’s deal with a classic tactic that is not evidence-based …
Stretching ain’t it
Weekend warriors and a lot of amateur athletes tend to believe that injury prevention is pretty much all about having a stretching regimen, and they are usually feeling guilty about not doing it enough. If I had a buck for every time I’ve heard someone say, just before a game of ultimate, “I should really do some stretching” … well, heck, I could afford to play ultimate for a living.
Lucky for them, they aren’t really missing anything important. As established elsewhere, stretching generally doesn’t work for the things people think it does,3 and it is particularly useless at preventing injury.4 Here are five ways to prevent injury that are a much better use of your time …
Train in the Goldilocks Zone: manage your training “load”
One of the few things we know for sure is that injury is linked to training “load”5 — how hard and quickly your tissues are challenged. So load management is one of the best overall strategies for preventing injuries. What “load management” mostly means is avoiding spikes and lulls in training and competition where possible … and when they do occur, be more cautious for a while. Train regularly and moderately, with only moderate increases in load.
That’s the tip of the iceberg on the topic of load management. It’s simple in principle, but the devil is in the details. In 2016, a panel of experts for the International Olympic Committee covered all of those details in an exhaustive scientific paper on this topic, “How much is too much?”6 Here are the main points they made, translated to plain English:
- There’s not enough research, surprise surprise, and what we do know is mostly from limited data about a few specific sports. But there’s enough to be confident that “load management” overall is definitely important.
- Both illness and injury seem to have a similar relationship to load — lots of overlap.
- Too much and not enough load probably increase the risk of both injury and illness. You want to be in the goldilocks zone! But the devil is in the details …
- Not everyone is vulnerable to high load, and elite athletes are the most notable exception: they are relatively immune to the risks of overload, probably because of genetic gifts. Everyone else gets weeded out!
- Big load changes — dialing intensity up or down too fast — are much bigger risks than absolute load. If you methodically work your way up to a high load, it may even be protective.
- “Load” can also refer to non-sport stressors and “internal” loads, which are legion. Psychology, for instance, probably does matter: anything from daily hassles to major emotional challenges, as well as stresses related to sport itself.
Most of the tips below are really just diving deeper into the implications of load management.
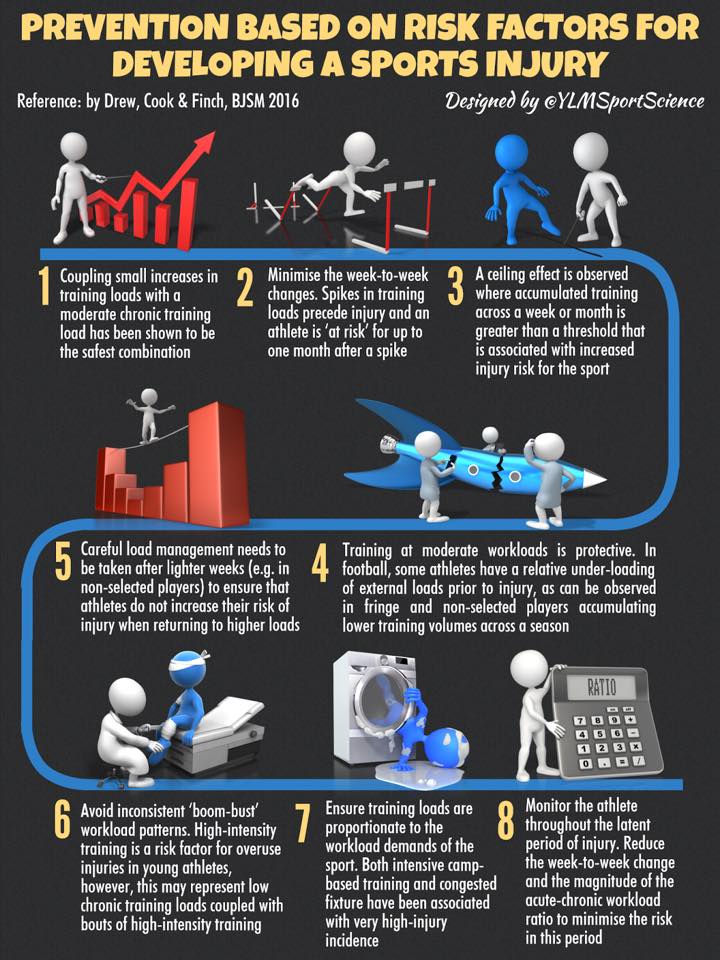
A fine infographic from Yann Le Meur (
Warm up
The best simple way to prevent injury is to warm up.78 Prepare for any intense activity by doing a similar activity less intensely. In other words, start slow! To warm up your tissues, you need metabolic activity: the heat causes physical changes in connective tissues that make them more pliable. Many more complex benefits arise from the stimulus of mild physiological stress. Mobilizations9 are an excellent warmup method, but really it’s just a matter of starting intense activities slowly.
Conversely, don’t overdo it. I’ve seen sports teams scrimmage for an hour before game time. I think that’s crazy: players go into competition not only warmed up but worn out. In competition, you can’t afford to give up any resources, and you only have so much juice in a day — no matter how fit you are. Athletes get hurt far more when they are fatigued than when they’re fresh.
And speaking of being tired …
Get your zzzleep
As just mentioned, fatigue is a major risk factor for injury. Sleep deprivation is an almost universally underestimated problem. It’s a major factor in chronic pain.10 It impairs athletic performance, getting more sleep boosts boosts performance,11 and injury rates and recovery are probably affected too.12
People who actually do get enough sleep are extremely rare, and of course actual insomnia is a common problem. Insomnia treatment is not as hard as people think, and it’s a great indirect injury prevention tip, something that is definitely relevant to performance and injury risk — but has nothing to do with what you’re doing before, during, or after workouts.
Cultivate coordination
Many traumatic injuries are probably caused by minor glitches in coordinating fast, powerful movements — an inability to sense and respond to traumatic forces at just the right time, either from lack of developed skill and/or fatigue. Creating coordination takes practice at complex and specific tasks (working within genetic advantages and disadvantages). But you can make some progress simply challenging yourself with a wide variety of activity and sensations, and coordination can be improved.13 For instance, a particularly long-term study followed a men’s basketball team for six years, tracking their injury rates in response to “classic proprioceptive [coordination]14 exercises” — which seemed to clearly reduce ankle sprains, and possibly more.15
Balance is one of the most basic elements of coordination, and isn’t much of a concern for younger athletes, but it becomes one for older adults — and even fit older people fall just as much as their less active counterparts. Fortunately, if you practice tasks that require balance, your balance will usually get better (as long as there’s no medical issue). And better balance means fewer falls.
Play smart, not hard
Many injuries are caused by excessive and mis-directed effort! That might seem like a bit of a no brainer, but people need to learn this. I certainly did. It is one of the great lessons of martial arts.
I remember the day I learned this lesson in ultimate, watching an older woman play. She seemed unlikely to be competitive — she was simply too old, and a little overweight. In fact, it turned out that she was the best player on the field that day, entirely because she was clever. I particularly remember how little she ran. Although there were certainly bursts of intensity, her effort was precise and savvy, and time and again she got the better of other players with only a fraction of the sweat.
One particularly important way of playing smart is to relax into intense challenges …
Chill out, man
Adaptability prevents injury, and rigidity is the opposite of adaptability. Relaxation is more psychological than golf. To purge rigidity from your system, you will have to go on a journey of self-exploration: most tension is emotional and protective. You won’t be able to relax and be “comfortable in your own skin” until you know yourself better. Meanwhile, you’ll get more injury prevention mileage.
Heed the signs! Painful “niggles” are a loud-and-clear sign of an increased risk of injury

It’s not an injury… yet.
You get a nasty knee twinge while you’re being sporty and physically intense. It’s nothing terrible, just a niggle really, not enough to stop you… but maybe you should stop? What if you knew that a twinge means that your risk of an injury just tripled?
No one knows that, unfortunately. Despite athletes being studied as much as lab mice, this warning sign — which would have immense value to the elite sports industry, if confirmed — has barely been touched by researchers.
But it has been touched now, by Whalan et al. They studied a bunch of soccer players to show that minor physical complaints — “niggles” — are probably clear warning signs of more serious athletic injuries.16 How clear? The complaints were linked to at least triple the risk of a more serious injury in the next week. 😲 Triple!
Speaking for myself… I am getting old enough now that I haven’t gone a day without a niggle, let alone a week, since about 2015. If I stopped for every niggle, I’d never do anything active at all!
I discuss this topic in a bit more detail in my book about muscle strains.
Part II: Collateral and re-injury prevention
Don’t underestimate the importance of prevention … after you’ve already been injured! After an injury, you should double-down on injury prevention.
The risk of re-injury and collateral injury is a significant factor in many cases of chronic pain. Minor re-injury can stop healing in its tracks, or at least slow it down. Injury “prevention” is therefore not just a way of keeping yourself from getting injured in the first place, but directly relevant to recovery from obvious injuries that have already happened. Double or triple your alertness and caution when limited by an injury, and bear in mind the risk of minor re-injury turning an injury into a chronic pain problem.
We’re not just talking about the risk of a second “oh @#$!&” moment, dramatically re-injuring your injury, although that can certainly happen: re-injury routinely occurs in small, sneakier ways. And every minor re-injury impedes recovery. Minor re-injuries can be so subtle that you aren’t even really aware that it’s happening — all you know is, you aren’t getting better fast enough. (Although it’s awfully hard to tell how fast is fast enough.17)
Good health care professionals are always considering the “aggravating factors” of their patients’ pain problems. What factors in patients’ lives are making the problem worse? What keeps people from healing? What adds insult to injury? In a sense, almost every “aggravating factor” is basically just a kind a re-injury. You could call them “micro” re-injuries.18
When you are trying to figure out why your injury isn’t healing, do not neglect this important perspective: could you be slightly re-injuring yourself regularly? Have you actually removed from the equation any forces that might be, even just slightly, hurting you again … and again … and again … ?
Injury déja vu: the risk of real re-injury
Obviously, injured parts are vulnerable. A classic example of re-injury is the ankle sprain. The anterior talofibular ligament in the ankle is the most commonly injured structure in the body — and undoubtedly the most commonly re-injured structure in the body. Once it is damaged, it is never the same again. The chances of having a second ankle sprain are way higher than the chances of having the first. Almost exactly the same is true of muscle strains ("pulled" muscles), one of the most common athletic injuries.
People also often continue doing the very same activity that injured them in the first place. Like me, for instance: for years, I had almost annual compression sprains of my thumb joint — a “thumb jam,” well known to rugby players — from playing ultimate.19 I was at great risk for re-injury because I kept exposing myself to the same dangers, and the thumb was so damaged that virtually any impact constituted a real hazard, flaring it up again for weeks.
The need to avoid re-injury might seem too obvious to even bother writing about. But the failure to do so isn’t just an amateur mistake made by people too eager to get back to normal after an injury. For decades, patients have often been encouraged to do so by professionals, to the point of serious risk. It’s been in vogue in physical therapy for a long time now to “mobilize” injuries as quickly as possible — probably too much in vogue. In the zeal to get people on their feet again ASAP, serious sprains — which are worse than fractures in some ways — are almost never put in a cast. Turns out that’s a mistake. A 2009 experiment published in the Lancet presents clear evidence that a full cast for a severe ankle sprain is superior to the almost universal practice of using braces and tubular compression bandages. The editors write, “This elegant study highlights the need for trials to address common problems.”20 In other words, it has not been common sense to make re-injury avoidance a top priority.
In many contexts, getting active makes complete sense — but doing it prematurely can be a disaster. You definitely have to consider the risk of re-injury when you are trying to heal.
Collateral injury: when you are hurt, you are at higher risk for completely different kinds of injuries
One of my massage therapy clients21 had a shoulder injury — an ordinary thing, no big deal, just a little rotator cuff lesion, a tear in the muscles around the shoulder socket. Unfortunately, it impaired her ability to catch herself when she tripped and fell. It is amazing — shocking, really — just how hard you fall when you aren’t able to catch yourself. She fell face first onto a curb, and fractured her jaw and facial bones severely … a much more grievous injury than the original shoulder injury.
This kind of thing is surprisingly common. Patients with injuries need to be wide-awake alert to the fact that you are more vulnerable when you’ve been injured!
Being injured is an unfamiliar state, and it’s the “weirdness” of that state — the new sensations, and limitations — that gets people into trouble. An injury basically induces poor coordination (some more than others). Just like a child needs to be warned to look both ways before crossing the street, injured people — especially if they’ve never been injured seriously before — need to be warned to be much more alert to potential dangers.
Masking symptoms
A major mechanism for re-injury is the overconfidence given by masking symptoms with medication. Pain killers and anti-inflammatories, when they are effective, can make you feel less vulnerable than you actually are.22 And that’s when you’re going to go too far and hurt yourself … again. And you may not even realize it, both because of the masking and because it doesn’t have to be serious re-injury to really slow down recovery.
“Masking symptoms,” especially with medications, is often maligned because it doesn’t “treat the root cause.” But masking symptoms can be a good idea, and it should not be eschewed just because it doesn’t have a real healing effect … because there are very few real healing effects! “Healing” is mainly about removing impediments to natural recovery, like stress on tissues. It’s not dictated by some mythical power to speed healing, but by a strong understanding of the nature of the problem and what pisses it off and impedes recovery. Focus on facilitating natural recovery, and don’t knock a little “symptom relief” along the way.
But, if you decide you need some symptom relief, you must exercise more cautiously.
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
- Quite a Stretch — Stretching science has shown that this extremely popular form of exercise has almost no measurable benefits
- Mobilize! — Dynamic joint mobility drills are an alternative to stretching, a way to “massage with movement”
- Healing Time — Can healing be hurried? Would we even notice if it was?
- The Functional Movement Screen (FMS) — The benefits of the popular screening system for athletes might be over-sold by some professionals
What’s new in this article?
Four updates have been logged for this article since publication (2002). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more
Like good footnotes, update logging sets PainScience.com apart from most other health websites and blogs. It’s fine print, but important fine print, in the same spirit of transparency as the editing history available for Wikipedia pages.
I log any change to articles that might be of interest to a keen reader. Complete update logging started in 2016. Prior to that, I only logged major updates for the most popular and controversial articles.
See the What’s New? page for updates to all recent site updates.
2020 — New section: “Heed the signs! Painful ‘niggles’ are a loud-and-clear sign of an increased risk of injury.”
2018 — Substantive science update, added a bunch about load management based on Soligard. Also merged another article about injury prevention into this one: “Collateral and Re-Injury Prevention” is now a major second part of this article.
2018 — New tip, “Train in the Goldilocks Zone,” based on Drew. Several other improvements.
2017 — Minor science update, a couple citation drop-ins for the introduction.
2002 — Publication.
Notes
- Bahr R. Why screening tests to predict injury do not work-and probably never will … : a critical review. Br J Sports Med. 2016 Jul;50(13):776–80. PubMed 27095747 ❐ “To date, there is no intervention study providing support for screening for injury risk.”
- Dorrel BS, Long T, Shaffer S, Myer GD. Evaluation of the Functional Movement Screen as an Injury Prediction Tool Among Active Adult Populations: A Systematic Review and Meta-analysis. Sports Health. 2015;7(6):532–7. PubMed 26502447 ❐ PainSci Bibliography 53719 ❐
The first review of the predictive validity of The Functional Movement Screen (FMS), with a predictably and resoundingly negative result based on mediocre data from 7 studies: “Based on analysis of the current literature, findings do not support the predictive validity of the FMS. Methodological and statistical limitations identified threaten the ability of the research to determine the predictive validity of FMS.”
See The Functional Movement Screen (FMS) for more information.
- Stretching is not a pillar of fitness: it doesn’t warm you up, prevent or treat soreness or injury, or enhance peformance, but it can cause injuries and (slightly) impair performance. It’s possible to increase flexibility, but the value of flexibility is surprisingy low, even for most athletes. Many key muscles are mechanically impossible to stretch in the first place. Stretch might help some kinds of pain, like muscle pain, but that’s quite speculative. There is no “advanced” stretching method that overcomes any of these limitations. See Quite a Stretch: Stretching science has shown that this extremely popular form of exercise has almost no measurable benefits.
- This article reviews several lines of evidence on the topic of stretching to prevent injury: Quite a Stretch
- Drew MK, Cook J, Finch CF. Sports-related workload and injury risk: simply knowing the risks will not prevent injuries. Br J Sports Med. 2016 May 10. PubMed 27166288 ❐
- Soligard T, Schwellnus M, Alonso JM, et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016 Sep;50(17):1030–41. PubMed 27535989 ❐
- Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. PubMed 19066253 ❐ PainSci Bibliography 56160 ❐
Research has shown for years now that good ol’ stretching doesn’t really prevent athletic injuries. So what does? Warmups that “improve strength, awareness, and neuromuscular control” might just do the trick. Practicing coordination and control, basically (see Panics et al). In 2008, Norwegian researchers compared injuries in over a thousand female footballers who participated in such a warmup for a season, to another several hundred who didn’t. Athletes who warmed up had fewer traumatic injuries and fewer overuse injuries. Moreover, the injuries they did have were less severe. Static stretching was not part of the warmup, but “active” stretching was (i.e. Mobilize!).
- Soligard T, Nilstad A, Steffen K, et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010 Sep;44(11):787–93. PubMed 20551159 ❐ PainSci Bibliography 54998 ❐
Researchers found that injury rates were significantly lower in soccer (football) teams that diligently performed warmup exercises (“The 11+”, a warmup program recommended by FIFA, which notably does not include stretching). On the one hand, there was not much difference between a little warming up (low participation) and a bit more warming up (average participation). But players and teams that did an especially good job of warming up (“twice as many injury prevention sessions”) got solid results: “the risk of overall and acute injuries was reduced by more than a third among players with high compliance compared with players with intermediate compliance.” That extra enthusiasm went a long way!
- Mobilizations are rhythmical movements that gradually expand your comfortable range of motion, providing your tissues with a variety of stimuli and stresses. The basic philosophy of mobilization is “use it or lose it.” It is a specific method of warming up that also cultivates coordination and relaxation. It’s similar to stretching, but with a lot less emphasis on pulling on tissues. For more information, see Mobilize!.
- Almost everyone needs to take sleep deprivation more seriously. We are used to thinking of insomnia as a symptom, but it can also be hazardous in itself in many ways. Chronic pain is probably aggravated by insomnia or even mild but chronic sleep deprivation. For more information, see Insomnia Until it Hurts: The role of sleep deprivation in chronic pain, especially muscle pain.
- Bonnar D, Bartel K, Kakoschke N, Lang C. Sleep Interventions Designed to Improve Athletic Performance and Recovery: A Systematic Review of Current Approaches. Sports Med. 2018 Jan. PubMed 29352373 ❐ Just getting more sleep at night “had the most beneficial effects” on athletic performance, compared to napping, sleep hygiene, and post-exercise recovery strategies for young athletes.
- Watson AM. Sleep and Athletic Performance. Curr Sports Med Rep. 2017;16(6):413–418. PubMed 29135639 ❐
- Panics G, Tallay A, Pavlik A, Berkes I. Effect of proprioception training on knee joint position sense in female team handball players. Br J Sports Med. 2008 Jun;42(6):472–476. PainSci Bibliography 56163 ❐
A general warmup with an emphasis on coordination has been shown to reduce athletic injury rates significantly (see Soligard, for instance). Perhaps it is the neuromuscular or proprioceptive training component of this that causes the effect. A 2008 experiment compared athletes’ with and without this kind of training. Those who did it had a greatly improved sense of joint position. In other words, they really knew where their joints were! “This may explain the effect of neuromuscular training in reducing the injury rate,” the authors concluded.
- Ingraham. Proprioception, the True Sixth Sense: The vital and strange sensation of position, movement, and effort. PainScience.com. 2254 words.
- Riva D, Bianchi R, Rocca F, Mamo C. Proprioceptive Training and Injury Prevention in a Professional Men's Basketball Team: A Six-Year Prospective Study. J Strength Cond Res. 2016 Feb;30(2):461–75. PubMed 26203850 ❐ The study showed significant reductions in ankle sprains, knee sprains, back pain … but “significant” is a highly problematic term, and only the reduction in ankle sprains was really persuasive. The athletes also got really good at the propioceptive control exercises themselves … for whatever that’s worth.
- Matthew Whalan, Ric Lovell, John A Sampson. Do Niggles Matter? - Increased injury risk following physical complaints in football (soccer). Science and Medicine in Football. 2020;4(3):216–224. PainSci Bibliography 51897 ❐
- People often believe that treatment X helped them to heal faster, but we can’t know that — because we never know how long it would have taken without it. If the effect is minor, only a bunch of careful testing can confirm it. For more information, see Healing Time: Can healing be hurried? Would we even notice if it was?
- Here’s one great example: I had a client with an exasperatingly tricky knee problem, a case of patellofemoral syndrome, a notoriously vague diagnosis that basically means “hurtin’ kneecap.” It was an overuse injury originally. Over the course of a long walk, her kneecap just started to hurt … and months later it was still hurting. What was keeping it going? I got nowhere with this client for several appointments, until one day when I was digging deeper into her story and learned that she had a habit of sitting at work with her knees bent sharply, her feet tucked well underneath her, a position that puts enormous pressure on the underside of the patella. Bingo — there was our “aggravating factor”! She was re-injuring herself all day long, every day!
- Ultimate is a Frisbee team sport, co-ed and self-refereed, with soccer-like intensity and usually the mood of a good party. Players tend to be jock-nerd hybrids: lots of engineers and scientists. Hippies invented the sport, but have mostly been displaced. I’ve been playing since 1997.
- Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009 Feb 14;373(9663):575–581. PubMed 19217992 ❐
- I was a Registered Massage Therapist with a busy practice in Vancouver, Canada, from 2000–2010, RIP. After that, science journalism and this website took over my career and they remain my sole focus today. See my bio.
- In fact, they can even do it when they aren’t effective: just the idea of symptom relief is all the excuse some people need to overdo it a little. “It’s okay, I can go a little harder and further — I’ve got some meds in me!
