Does Massage Increase Circulation?
Almost certainly not in a clinically important way, and definitely not as much as even a small amount of exercise

Massage therapists have long claimed that massage “increases circulation,” and this is one of the basic reasons it’s supposed to be good for us. The profession’s faith in the power of circulation boosting has remained strong for decades, and it’s a microcosm of a broader phenomenon: all kinds of alternative medicines supposedly help people by boosting circulation one way or another. It’s a sales bullet point for a dizzying array of products, from TENS machines to arnica creams, but nowhere is it touted more proudly or consistently than in the world massage therapy.
Any discussion of the physiologic effects of massage on the human body emphasizes the idea that much of the benefit is dependent in large part on the reflex and mechanical effects of massage on the circulation.
Wakim et al., 1949, Archives of Physical Medicine & Rehabilitation
While it may seem common sensical, this is the most glaring of several common myths about massage therapy, a classic careless belief with a premise that has never been validated. Although massage probably does sometimes modestly boost circulation — in some specific ways, depending on how you define it — it’s mostly too little and too erratic to matter, especially when compared to even light exercise. The relaxation that we expect from any decent massage deepens the problem: it actually shunts blood into the core, away from the muscles, but “boosts colon circulation” isn’t advertised by anyone.
Stimulating skin and muscle may have medical benefits, but it’s unlikely that they have anything to do with the circulatory system.
This is not an anti-massage article
It’s not all debunking! I will discuss three specific contexts in which the claim of increasing circulation could be more true and/or meaningful. But massage does not have to boost circulation to be awesome: there are lots of other ways it might help people. I loved working as a massage therapist, I have paid for massage therapy for myself regularly for almost 25 years, and this website enthusiastically recommends massage therapy to a massive audience — thousands of people every single day come away from this website thinking, for many reasons, “I should probably book a massage.” The only thing I’m criticizing here is one old idea about why massage therapy is a “fantastic experience.” My only motive in writing this is to understand and report as honestly as possible.1
I’ve been an MT for 27 years. I love what I do. I don’t find this kind of information threatening at all because I’m not running a circulation boosting business.
The elephant in the room: circulation is mainly about exercise
It mostly doesn’t really matter if massage increases circulation, because even a modest boost would be clinically trivial, dwarfed by the effect of almost any amount of exercise. The need for fuel — metabolic demand — is the main driver of circulation. Pressure on muscles is not.
And it’s worth emphasizing the obvious: exercise isn’t healthy because it boosts circulation. If you could somehow push blood around the body faster than normal without exercising — without high metabolic demand, without a high heart rate — it wouldn’t do anything for you.
Massage therapist Jamie Johnston has a good story about how he came to this realization. show story
Jamie Johnston, RMT, from his article, Altered Skin Colour And Circulation, Result Of Massage Or Nervous System?
I was working with a hockey team and one of the players had an episode in the summer which required him to be on blood thinners. I was super worried that if I did any massage I’d have an adverse effect on him, so I approached one of my teachers to ask if massage was contraindicated and what I should do as I was worried about the increase of circulation with his condition.
My teacher simply looked at me and said: “you’re not going to increase his circulation any more than him playing hockey!”
It was like a light bulb of astonishment went off, I wish I had a picture of my face.
What does “increase circulation” actually mean?
The amount of blood in circulation — blood volume — is fastidiously regulated by the body and only meaningfully drops below optimal levels if we are dehydrated enough to be quite thirsty.2 Hopefully no one has ever believed that massage actually makes more blood, so what does “increase circulation” even mean? There are really only two main options:
- Temporarily increase it in one area at the expense of another. In a closed system, getting more blood in one place means it has to be borrowed from somewhere else.
- Increase the speed at which it circulates. This is what happens in exercise: the heart pumps faster, because the goal is to deliver oxygen to tissues as speedily as possible, get it back to the lungs to be recharged, and then back out to the tissue again. Without an increased rate of respiration, blood flow rate is largely irrelevant.
These are not the only conceivable definitions of “improved circulation,” but they are the main ones. There will be more about the details of hemodynamics and the meaning of “circulation” below.
Imagine strangling the circulation in your arm with a tight tourniquet. Only a trickle of blood makes it past in either direction. The blood that was already in your arm cannot escape; it stagnates until it’s drained of the heat and oxygen it brought from the core. When you finally release your arm, you feel a warm rush of blood, and there is no question in your mind: in that moment, circulation to your arm has definitely increased! It feels like it’s “filling up” an empty arm, but of course the volume hasn’t changed, it’s just a swap: fresh, hot arterial blood quickly flushing out the stale, cool blood.
What increased was the rate at which oxygenated blood flowed past the cells of your arm. And that is mainly what is meant by increasing circulation.
Reflex versus mechanical effects, and the other elephant in the room: relaxation!
Circulatory effects of massage are mainly assumed to be either:
- a neurologically mediated reflex response
- a matter of pure plumbing, the hydraulics of moving fluids around
The idea of reflex effects is often trotted out to try to save the claim — neurology is so complex that it can seem plausible to attribute almost anything to it — but it doesn’t much matter how circulation is increased if it isn’t increased. One thing at a time.
The reflex effect to rule them all is probably relaxation, which is the other elephant in the room of this topic. (That’s two elephants in one small room now.)
When we panic, blood floods into the muscles to prepare us for action — a robust system that evolved long ago.3
When we relax, the opposite happens: powerful neurological and hormonal forces divert blood away from our muscles and towards the internal organs and skin (and the opposite when adrenaline is pumping).45
If massage is going to increase circulation to any muscle tissue generally, it is going to have to fight that effect to do it. While it’s not inconceivable that circulation could increase locally despite a general trend in the other direction, it would certainly be swimming “upstream,” a weaker and briefer effect. Relaxation probably dominates the equation.Intuitively speaking, most of my clients tend to sleep or enter a resting state while receiving a massage. I’m the one moving around the table and doing the work. If there’s one person in the room who has “improved” circulation, it would be the therapist.
If clients want to “improve circulation,” maybe they should give me a massage instead. Or better yet, go take a walk around the mall or workout at the gym.
Nick Ng, BA, CMT, publisher of Massage & Fitness Magazine
Red skin: the most obvious (and underwhelming) example of a reflexive circulatory shunt
Massage makes the skin flushed and warm. This is superficial (cutaneous) hyperaemia: capillaries in the skin respond to mechanical stimulation by dilating. Blood is hot, so the skin gets toasty.
You can also get this shallow effect with a little Tiger Balm, which is literally just a minor skin irritant.6 (Ironically, tigers hate Tiger Balm. Just sayin’.)
And although it’s not a lot of blood moving around, guess where it comes from? It’s probably diverted from underlying muscle!7 You could use that evidence to argue that massage reduces circulation to musculature.
If you’re keeping score, that is now two ways in which massage may actually reduce circulation to muscle: shunting to the core with relaxation, and shunting to the extreme periphery with skin stimulation.
The CPR thought experiment
In cardiopulmonary resuscitation, firm and rapid chest compressions are used to passively pump the heart, literally squishing it repeatedly to simulate a heartbeat. This is effective. It increases circulation, enough to save lives. And it even does so in a massage-like way: applying pressure with the hands. Very hard, very fast, in one spot. But still a bit massage-like.
If chest compressions can increase circulation, it demonstrates a principle: you can move blood around with your hands. So maybe other massage techniques have a similar effect? Not nearly enough. Chest compressions are probably an exception that proves the rule that most massage cannot move much blood. If other kinds of massage were anywhere near as good at “increasing circulation,” presumably they would have replaced or supplemented chest compressions in CPR.
Obviously this is a bit whimsical — surely no one thinks that massage would ever save someone from a stopped heart — but it is a good little thought experiment. If you imagine trying to save someone from a heart attack with massage, it’s obvious that you’re just not going to move much blood around; if you really wanted to “increase circulation,” you would do it with chest compressions. Hat tip to C.L.G. for suggesting this amusing perspective.
More hemodynamics — what is “circulation” and what controls it?
The main point of “circulation” is the delivery of oxygen-rich blood to tissues via capillaries and the removal of metabolic waste products, and so “circulation” can broadly be defined as anything that affects those processes. The technical term for the laws that govern circulation is hemodynamics, and it’s fantastically complex in its details.8
But it’s mainly about blood pressure and the major variables that affect it, because circulation is mainly about pushing blood through capillary beds. Capillaries are fantastically tiny things, cellular scale tubes; by the time blood gets there, it is moving through vessels so tiny that only single red blood cells can pass. Blood has to be continuously shoved through trillions of these teensy bottlenecks, and so it all comes down to the variables that affect that constant pushing and shoving.
And yet massage reduces blood pressure, because it’s relaxing! Hmmm. At the highest level, it’s implausible that relaxing massage can help people push blood through capillary beds. But details…
“Blood pressure” as we normally mean it is specifically the pressure of blood against the walls of larger blood vessels. It is affected mainly by how hard and fast the heart pumps, by blood volume, and by peripheral vascular resistance — and each of those in turn is affected by several more variables, for a great many variables in total, some of them downright exotic (the nitty gritty of rheology).
On the one hand, that means there are a lot of potential ways for massage to theoretically affect circulation. On the other, it’s also an awful lot of stuff that controls circulation that has nothing to do with the relatively brief, minor inputs of pressure on soft tissues. Trying to affect circulation with a partial, temporary grip on a couple of the variables is probably like trying to change a river by sticking your hand in it.
Schnell, schnell, blut! Accelerating circulation
Enough context and speculation already! Where’s the science beef? Does massage speed up circulation? Do muscles in particular have more blood flowing through them? This isn’t something anyone should try to guess at: it has to be tested. And it has been tested, now and then, over the decades.
A 1954 experiment by Wakim et al. seems promising … until it sinks in that they only found noteworthy circulatory increases with extremely strong, stimulating massage — the kind of massage few people want.9 A more peaceful and typical massage style had only tiny effects in their study. A 1974 experiment by Hovind et al. had similarly divided results: no change with typical, kneading massage (petrisssage),10 and a bit of a boost with a much rarer and more stimulating type of massage stroke.11

This is the only kind of massage that has ever been shown to increase the rate of blood flow in arteries, and it probably does it by either irritating muscles enough to cause an inflammatory reaction, and/or by provoking a fight-or-flight response.
So you might get some temporarily increased circulation from massage so vigourous that most people wouldn’t want it. (And you could probably get a much better circulatory boost from a 10-minute walk — and then you could still go for a more pleasant massage.)
Much more recently, and with a newer method, Shoemaker et al. used doppler ultrasound to measure the effect of common massage techniques on a small (forearm) and a large (quadriceps) muscle mass. They found even less of an effect on circulation:
The results indicate that if an elevated muscle blood flow is the desired therapeutic effect, then light exercise would be beneficial whereas massage would not.
So case closed? No, not quite
Not much in musculoskeletal medicine is truly settled. This is yet another example of a topic that simply hasn’t been studied enough (true of nearly everything in musculoskeletal medicine). Specifically, no one has ever really used a good enough method of measuring what matters, and the conclusions about circulation — both positive and negative — have only ever been inferred from that imperfect data.12 Even if those studies were otherwise perfect, they probably still wouldn’t be good enough.
So I don’t think it’s possible to reach a conclusion, and calling circulation boosting a “myth” might be a bit premature on my part. I might change that in the future.
And yet the evidence so far is not useless, and it doesn’t look great for the claim. There’s also a counter-argument that the Doppler ultrasound method is probably good enough, and its results are unlikely to be all that different from more direct measurements. And the myth status isn’t based solely on the evidence, but also because that exercise elephant is still in the room: until I see good data that says otherwise, my mind is made up that a modest temporary boost in circulation is not clinically important even if it happens. A temporary increase in blood flow simply doesn’t matter much in tissue that had basically normal circulation to begin with.
Evidence in favour of massage improving circulation
Franklin et al. from 2014 is a good example of a study that points the other way.13 It is obviously at odds with my skeptical bias, so I will avoid dismissing its findings out of hand, and acknowledge right away that, yes, this definitely constitutes scientific evidence that massage is good for circulation in at least one specific way.
But I do have problems with it. 😉
The experiment showed not only that typical Swedish massage increased the “responsiveness” of blood vessels for up to a day, but that it did so throughout the body — in the arms, specifically, when only the legs were massaged.14 Their conclusion, translated: in some healthy young couch potatoes, when blood vessel function has been impaired by wicked workout soreness, massaging their legs seemed to improve it in their arms.
More functional blood vessels seems like a good thing! But note that it isn’t “increased circulation” per se, just one of many biological factors in circulation. It would be a leap of logic to characterize this as evidence that massage “increases circulation,” especially given other evidence showing no significant effects on actual blood flow (the most obvious and direct measure of “circulation”).
But, if true, it is an interesting and happy result.
Unfortunately, I don’t think this is a good study or paper, and I simply don’t trust the authors or their conclusions. First of all, the lack of a true control group here isn’t just a “limitation,” as the authors acknowledged, it’s closer to a deal-breaker. And there are many red flags and a through-the-roof risk of bias shining through in many ways in the text.15
In any event we have yet another case of the evidence sitting in the deep shadow of exercise. Even if the results can be replicated, does it really matter if massage does this when it’s super plausible that almost any amount of exercise also has a dramatic systemic effect on flow-mediated dilation? Not in my opinion.
Increasing circulation in people who can’t move (or can’t move much)
Not everyone can exercise to boost their circulation, but people with severe illness, disability, or even paralysis have a genuine medical need for it. These patients represent only a tiny fraction of the business of massage therapy, so this is only of academic interest, but it is worth a little discussion.
The importance of circulation to tissue health is highlighted by a problem like bedsores or pressure ulcers, which do not take all that long to form in people who are substantially immobilized. Ask any nurse. They are underway within a couple hours, and even people who log serious time working in chairs are probably flirting with pressure sores — it’s just that they are easily prevented with relatively little movement.
Or massage? This has been studied… sort of. A 2015 review found “no studies eligible for inclusion” — not a single one! The ultimate “garbage in, garbage out” review.16
I bet that massage can prevent and treat pressure ulcers… but so can simply relieving the pressure. Which is easier, and what nurses do. “Changing position” is the “exercise” of this situation — and it’s enough. By the time you’ve moved a patient enough to reach a pressure ulcer, it has probably already been effectively treated.
Similarly, patients who are disabled but mobile enough to avoid pressure ulcers themselves are probably also mobile enough to increase circulation more than massage. To the extent that people are capable of any movement or exercise, it is probably always better at increasing circulation. Hell, laughing is probably better for circulation than massage.
Venous insufficiency
Venous insufficiency is blood literally pooling in the veins of the legs, primarily because of the failure of one-way valves that should be stopping blood from being pulled back to the feet. It’s what causes varicose veins, plus causing uncomfortable swelling and a bunch of other complications and risks. It’s an aging problem, exacerbated by poor fitness, and it is the most obvious common clinical scenario where someone could really use “increased circulation.”
One does wonder how massage is supposed to make those valves work better, but it still seems worth testing.
The only science on this topic I’m aware of is a low quality 2012 study with high risk of bias (published in Complementary Therapies in Medicine).17 They compared the effects of both massage and minimal exercise therapy on poor circulation (venous insufficiency) in post-menopausal women. Superficially it looks like a good news story for massage, and in some ways it is, but there are a lot of caveats.18
There were a lot of measures of success, and none changed all that much. The phrase “damned with faint praise” comes to mind, as it so often does in massage science.
Some of the measures also seemed barely useful. If I got that much massage, I’d probably feel like my “quality of life” had improved too! But I’m not sure that would have much to do with a small improvement in my venous insufficiency.
And it was really a lot of massage (expensive in the real world).
And the pure “kinesiotherapy” (movement) treatment was super basic — this control group barely did more than wiggle their toes and clench their thighs, so it’s hardly surprising that they didn’t improve much. You’d only be that minimalistic about it if you were so disabled that you had no other choice. I wish the study had included a third group doing more exercise, perhaps a half hour of brisk walking per day, or even ten minutes. There’s an excellent chance walkers would have performed just as well or even far better than massage. And walking is notably a lot cheaper than massage (and also an impressively effective form of exercise, delivering substantial health benefits efficiently19).
Most people with venous insufficiency need more activity, not massage therapy.
Danger, Will Robinson! Dangerous clots! Deep vein thromboses and pulmonary emboli
If blood gets stagnant enough, clots will form. In humans, this mostly happens in the deep veins of the calves, a deep vein thrombosis (DVT). This impairs circulation and causes swelling, redness, and pain when the blockage is bad — but they can also be totally asymptomatic. It’s surprisingly common for people to just carry clots around in their veins for years, no big deal.
Disturbingly, there is really no way to be sure someone does not have a big ol’ DVT lurking in their calf. In general, asymptomatic ones are less dangerous, but that’s only a rule of thumb.
DVT treatment is mostly about keeping the clot from getting any bigger (with blood thinners; irrelevant to massage) and minimize the risk of it breaking loose and getting stuck in the lungs: a dangerous pulmonary emboli. Which is extremely relevant to massage.
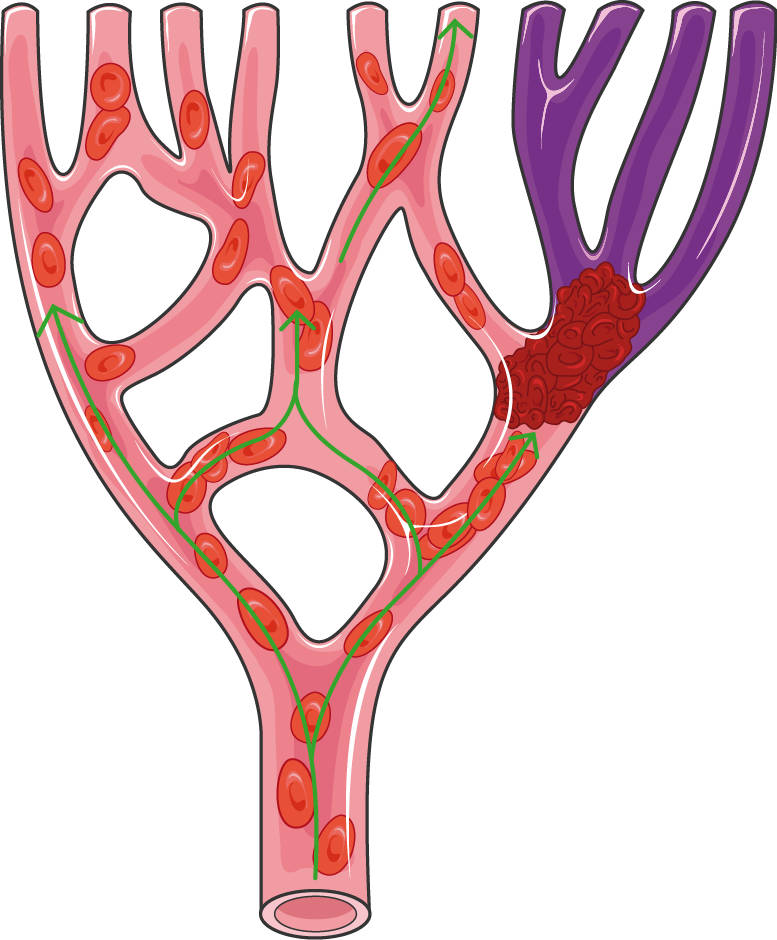
A blood clot blocking circulation to branching downstream veins (purple), as occurs in pulmonary emboli.
Calf massage when DVT is suspected is like playing Russian roulette
Clots that break loose will be swept downstream by the circulation until they finally get trapped by the filter of the lungs,20 with symptoms ranging from trivial to deadly. Sudden chest pain, breathlessness, fast breathing, pounding heart, and coughing are the symptoms that both clients and massage therapists should be alert for during and immediately after calf massage, and on first getting up from the table.
Yes, this does actually happen: there are several case reports.21 22 23 24 25 26 It doesn’t happen a lot for several reasons. Calf massage isn’t super popular or common in the first place, and strong calf massage even less so, because calves also tend to be quite sensitive to strong pressure — and people with substantial clots really aren’t going to want their legs massaged firmly. Swelling and redness will be good warning signs not to mess with that calf!
Do we have more robust evidence that the danger is real? Something beyond case reports and reasonable speculation? No — and we probably never will.27 But if I returned to work as a massage therapist today, I would refuse to massage the calves of anyone with a history of DVT, a recent leg trauma, any older patients who are obese and sedentary, or pregnant patients.
The trouble with mild cases — “silent but deadly”
It’s a basic rule of pathology: for every severe case, there are many minor ones. So, for every serious and obvious case of large clots, there are surely a batch of smaller ones… but which can still cause permanent lung damage. “Minor” pulmonary emboli are a lot like “minor” strokes: you don’t really want to kill off any tissue in your brain or your lungs!
Minor clots are a lot harder to avoid, because they aren’t obvious, and they can and do occur in people who are not high-risk.
And the consequences are harder to detect, too — almost impossible, I would argue. The symptoms of pulmonary emboli can be weirdly minor. Many of the smaller pulmonary emboli simply cause no symptoms at all. Even fairly large ones can cause only a bit shortness of breath and minor chest pain — symptoms that can and will be shrugged off by many people.
This is why the case studies I cited above are likely the tip of the iceberg. Even the really dangerous cases are probably under-reported. In many cases the link to massage won’t be made in the first place. Even when doctors know that a pulmonary embolus happened, they often won’t know how it happened. And the more subtle the symptoms, the harder it is to connect them to a massage.
Unfortunately, it’s highly plausible that quite a few people get off massage tables with lung damage.
“Objection! This clotting stuff has nothing to do with real/competent massage therapy”
I have heard this defensive, circling-the-wagons reaction to this clotting hazard a few times. I take a dim view of it: I think it’s naive, and puts pride and professional promotion ahead of concern for patient safety (and intellectual curiosity). I am afraid these horror stories really do have something to do with “real” massage therapy. (It also doesn’t have to be about “real” massage therapy to be useful information.)
Of course the best massage therapists are aware of the risks of massaging someone at high risk for DVT. But surely competence also means they wouldn’t object to promoting awareness of a serious safety issue in their profession? And surely the best also should be aware of how subtle the warning signs can be?
Unfortunately, not all massage therapists are competent and well-trained, and even competent and well-trained massage therapists may not be as aware as they could be. Some of this information was inspired by a question from a professional massage therapist who did not know that this was possible. Many other massage therapists have asked me similar questions, clearly indicating that they do not understand the biology and the risks well. And a real massage therapist actually told me once that breaking up blood clots is one way that massage can “increase circulation,” and she wasn’t joking. Technically true! Also dangerously ignorant — which follows from the prevalence of anti-scientific and magical thinking in massage therapy.28 When people believe in energy medicine, they aren’t going to be as interested in the real kind.
In any case — even if massage therapists are so awesome that they don’t need any reinforcements of their education, ever — this is also useful safety knowledge for non massage therapists who love massage and perform self-massage and partner-massage.
Claudication, pinching of blood vessels, and thoracic outlet syndrome
Arterial narrowing can cause “claudication,” the pain of impaired circulation, which is usually a symptom of peripheral artery disease (atherosclerosis), but there are several other pathological causes, like clotting. Hopefully no massage therapist has ever claimed to be able to treat or even compensate for vascular diseases, especially if it’s severe enough to cause claudication.
But claudication can also be caused by physical arterial impingement — pinching by other anatomical structures — and it’s more plausible that massage might be able to help in some cases like this. If it can, it would be a legitimate example of massage increasing circulation (even though it’s not really what is usually implied by that idea).
There is, however, just one clinical scenario where massage has much potential to treat claudication. There is a thick web of nerves and blood vessels that pass from the neck to the arm. Impingement of this bundle is called thoracic outlet syndrome. Most TOS symptoms are probably due to pressure on nerves, but some cases are dominated by vascular entrapment, usually by bony abnormalities, overgrown muscles, or both.29
Massage only has potential to help if the muscles are involved in a particular way: enough chronic contraction to cause a problem, but not so extreme that it’s a lost cause. For instance, if the scalene muscles are compressing vessels because they have grown strong and thick over decades,30 massage is not going to make them smaller.
“Enough contraction to cause a problem”? This is an unclear predicament: not pathological cramping and spasticity, but still something serious enough to eventually cause trouble in an otherwise healthy person. Why muscles might do that, and what would make them stop, is mostly a blank spot on the map of medical science.31 Massage might help, but no one really knows, and it probably varies a lot from case to case.
Bottom line: no one knows, but it’s possible that massage can reduce vascular compression in some cases of TOS.
Trigger points and ischemic pressure (or highly localized flushing)
“Trigger points” are the name given to the unexplained sore spots that practically everyone suffers from — just little aching, sensitive patches of tissue. Although their explanation is controversial, no one denies that they exist and are a source of considerable misery. Massage is the most popular and “instinctive” treatment approach — it often seems like they can be rubbed away. The evidence that massage is truly effective is scanty and sketchy and simply inconclusive.32
According to conventional wisdom, trigger points are tiny spasms that become stagnant:33 oxygen starved and polluted with the accumulating waste products of muscle contraction.
Pressing and holding a trigger point is called ischemic pressure or blanching, and it’s the method of trigger point treatment used by most professionals. “Ischemia” is an inadequate blood supply to tissue. For an easy demonstration, just pinch your fingernail: it will go white around the pressure. That whitened tissue will rapidly become ischemic. When you release the pinch, assuming your heart is beating, the blanched tissue will quickly turn pink again as the blood returns to the tissue (re-perfusion).
The same thing occurs to some extent in the deeper muscle tissue when you press firmly on a trigger point. Why would you treat ischemia with more ischemia? Hopefully, swampy tissue fluid is pressed out of the trigger point … and then, hopefully, it refills with fresher, cleaner, more oxygenated blood. This highly localized tissue fluid flushing is one possible way that this might be effective (if it ever is).
In theory even a very brief application of pressure should be enough to squeeze the stagnant tissue fluids from a trigger point,34 but the common practice is to press and hold a trigger point for an arbitrary 20 seconds or more, and sometimes professionals prefer to apply pressure for much longer (2-3 minutes). There’s no clear justification for such long holding except a very basic “more is better” impulse.
Trigger points could be one of those biological situations where an effect on circulation might be both obscure and yet meaningful and relevant to massage therapy as many of us know it (since kneading stiff/sore spots is pretty much a staple of massage, whether it’s branded as “trigger point therapy” or not). If the tissue fluids in trigger points are stagnant, as suggested by Shah et al., then there is a greater need for and sensitivity to flushing, and it’s also possible that mere exercise won’t do the trick. You can dramatically increase net blood flow rate through a muscle — lots more blood being pumped through the arteries than baseline — without necessarily overcoming local restrictions.35 So it could make sense to vigorously massage an entire muscle, casting a wide net, hoping to flush whatever trigger points might be present in a way that exercise actually might not be able to do.
We are truly in the realm of speculation here. Despite that, I think this is probably the most promising example of a way in which massage might actually “increase circulation” in a way that matters.
What about lymph? Don’t forget the lymph!
Lymph is the clear fluid that circulates in a completely separate system of vessels, a mirror image of the circulatory system. The lymphatic system is primarily responsible for draining off excess tissue fluid and putting it back into the main circulatory system, passing it through immune system checkpoints along the way — the lymph nodes. The system is not pressurized: lymph is moved entirely by the mechanical stimulation of movement and muscle contraction.
There is a specialized massage technique — manual lymphatic drainage — which claims to be able to stimulate lymphatic circulation by triggering subtle reflexes that move the lymph along. It is widely believed that this is a vital service for some patients with serious lymphatic stagnation.
Even if it works, it’s a bit exotic and wouldn’t count as “increasing circulation” in the sense that most massage therapists mean it, so I won’t go all the way down this rabbit hole (maybe in another article someday). It is definitely possible that MLD is effective and, if so, it would count as a rather specialized case of increasing circulation, but the limited and mixed evidence36 doesn’t exactly inspire confidence, especially given some notably negative examples, pulling down on the average measured effect.373839
And there’s still that pesky exercise elephant in the room: while it is completely plausible that massage can move lymph around, it probably can’t do it as well as exercise, or no better40 … and it definitely cannot do it as cost effectively.
cerebrospinal fluid and craniosacral therapy
Cerebrospinal fluid is the fluid that surrounds and cushions the brain and spinal cord. It “circulates” sluggishly, pumped mainly by the movement of breathing.41 The belief that CSF circulation can be stimulated or manipulated is one of the classic tropes of the massage world, and specifically it is the central claim of craniosacral therapy (CST). It is not what massage therapists generally mean when they say that they can “increase circulation,” but it is an additional feather that many like to put in their cap.
CSF probably isn’t ever “stagnant” in the first place; there are no common or relatively minor problems that are attributed to it by any expert (outside the world of CST). CST is a solution to a problem that doesn’t exist. This is a stark contrast to, say, manual lymphatic drainage, which may or may not work, but is at least intended to help with a specific medical problem (lymphedema, swelling in a limb).
But for the sake of argument, let’s say that people actually do need to have the circulation of their CSF stimulated once in a while. Even in that case, it’s fantastically implausible that subtle physical manipulations could ever fix CSF stagnancy, not even for a few minutes, never mind hours or days. CST supposedly affects CSF circulation primarily by manipulating the bones of the skull — which cannot actually be moved,42 and which indeed do not even make way for dangerous internal swelling.43
And yet again, and one final time in this article: the effect of movement and exercise is probably much greater than anything a massage therapist can do with their hands.
Virtually the only thing CST is good for is that it is a relaxing touch therapy. For more on this topic, see Does Craniosacral Therapy Work? Craniosacral therapists make big promises, but their methods have failed to pass every fair scientific test of efficacy or plausibility
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the Internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
The major myths about massage therapy are:
- Massage increases circulation.
- “Tightness” matters. The three most common words in massage therapy — “you’re really tight” — are pointless.
- Massage detoxifies. It’s actually the opposite, if anything.
- Massage patients need to drink extra water to “flush” the toxins liberated by massage.
- Massage treats soreness after exercise. Studies have shown only slight effects.
- Massage reduces inflammation. An extremely popular belief based mainly on a single seriously flawed study.
- Fascia matters. The biggest fad in the history of the industry.
- The psoas muscle is a big deal. The most overhyped single muscle.
- Massage stimulates endorphins (natural opioid) and reduces cortisol (stress hormone). They do not.
- “Trigger points” are evidence-based. Actually, the science is seriously half-baked.
- Massage therapists have spooky palpation skills. No, it’s just ordinary expertise… and misleading.
The complete list of dubious ideas in massage therapy is much larger. See my general massage science article. Or you can listen to me talk about it for an hour (interview).
And massage is still awesome! It’s important to understand the myths, but there’s more to massage. Are you an ethical, progressive, science-loving massage therapist? Is all this debunking causing a crisis of faith in your profession? This one’s for you: Reassurance for Massage Therapists: How ethical, progressive, science-respecting massage therapists can thrive in a profession badly polluted with nonsense.
Other articles about massage and circulation (all by massage therapists):
- Does massage increase circulation? A clear, concise review of the topic by Alice Sanvito, LMT.
- Altered Skin Colour And Circulation, Result Of Massage Or Nervous System? by Jamie Johnston, RMT.
- Can Massage Increase Blood Circulation? by Joseph Muscolino. Some detail about the challenge of measuring circulation experimentally, plus some other good perspective.
- 5 Myths and Truths about Massage Therapy: Letting Go without Losing Heart, by Tracy Walton, MS, LMT. Boosting circulation is one of the five myths covered by this solid article.
- Flushing Out Myths, by Keith Eric Grant, PhD, more about flushing toxins than circulation, but relevant.
What’s new in this article?
Nine updates have been logged for this article since publication (2019). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more
When’s the last time you read a blog post and found a list of many changes made to that page since publication? Like good footnotes, this sets PainScience.com apart from other health websites and blogs. Although footnotes are more useful, the update logs are important. They are “fine print,” but more meaningful than most of the comments that most Internet pages waste pixels on.
I log any change to articles that might be of interest to a keen reader. Complete update logging of all noteworthy improvements to all articles started in 2016. Prior to that, I only logged major updates for the most popular and controversial articles.
See the What’s New? page for updates to all recent site updates.
2021 — Science update. Added a citation to Sheng et al. about the excellent fitness bang-for-buck delivered by walking.
2021 — New and upgraded citations of case studies of massage dislodging blood clots and causing dangerous pulmonary emboli. There are now six interesting summaries of these alarming stories.
2020 — Proofreading.
2020 — Added new section about cerebrospinal fluid circulation and craniosacral therapy, and another one about hemodynamics and the variables that affect pushing blood through capillary beds.
2020 — Added new section about deep vein thrombosis.
2019 — Added a new citation (Munk) that reduces my confidence in the available scientific evidence on this topic: it may be closer to “inadequate” than “negative.” My conclusions have been softened accordingly.
2019 — Added a section about ischemic pressure: highly localized “flushing” of tissues. Elaborated on the plausibility of scalene hypertrophy. Added an aside about levels of confidence in myth-busting.
2019 — Added a section thoroughly reporting on Franklin et al., which challenges my skeptical bias. Also added a fun quote.
2019 — Added citation about the effect of relaxation on circulation. Made it clearer that this is not an anti-massage article. Added tourniquet example to help explain circulation “increase.” Added a new section, “The CPR thought experiment.” Fixed several typos.
2019 — Publication.
Notes
- As always, my allegiance is to learning: I want to undertand and report how things actually work (or don’t.) That’s it. I don’t care if massage does or does not increase circulation. What I do care about is whether this old idea is true or false… and, so far, it seems to be mostly false, or at least misleading and trivial. If new evidence emerges that persuades me I am wrong, I’ll be just as eager to report that. Meanwhile, I am going to carry on loving massage no matter what, as I always have.
- Chronic mild dehydration wouldn’t be enough, even if it was actually a thing, which it’s not. See Water Fever and the Fear of Chronic Dehydration: Do we really need eight glasses of water per day?
If you’re a zebra being chased by that lion, you have to run for it. For us vertebrates, the core of the stress-response is built around the fact that your muscles are going to work like crazy.
Why Zebras Don’t Get Ulcers, by Robert M Sapolsky, 10
- Gordan R, Gwathmey JK, Xie LH. Autonomic and endocrine control of cardiovascular function. World J Cardiol. 2015 Apr;7(4):204–14. PubMed 25914789 ❐ PainSci Bibliography 52427 ❐ Gordan et al.:
during the ‘fight or flight’ response the sympathetic nervous system causes vasodilation in skeletal muscle, but vasoconstriction in the skin.
And the reverse when relaxing, of course. Control of the cardiovascular system is very complex, so no one citation is enough to completely support this point. But there is also no great need for this point to be rigorously supported: I’m not going out on a limb claiming that fight-or-flight boosts circulation to the muscles to prepare for urgent action, and that relaxation does the opposite. This is basic biology, neither extraordinary or controversial. However, it is a key point in the article, so I’ve provided this reference, which is a dense academic tutorial.
Massage therapist Alice Sanvito explains this in more detail in her own excellent review of this topic:
The sympathetic “fight or flight” nervous system diverts blood away from the skin and internal organs and towards the muscles. The parasympathetic “rest and digest” nervous system diverts blood away from the muscles and towards the internal organs and the skin. Since massage tends to relax people, it is probably safe to assume it is downregulating the sympathetic nervous system. So, what we were taught about massage increasing circulation, especially to the muscles, was probably wrong, but what we were taught about the sympathetic and parasympathetic nervous systems was probably correct, as far as we know.
- Ointments and balms like Tiger Balm, RUB A535, or Deep Heat are not really “hot,” but they do have two things in common with heat — they both feel hot, and they both cause superficial capillaries to open up as wide as they can. All these products contain a chemical irritant or rubefacient (and there’s your word-of-the-day). Rubefacients feel hot because they give you a mild chemical burn! Capsaicin is a classic rubefacient — it’s the stuff that makes chilli peppers spicy, on your tongue or your back. They piss off your skin, in other words. That’s the only sense in which a rubefacient is heating anything. The product name “Deep Heat” always makes me roll my eyes, because a more truthful name would be Shallow Irritation! “Chemicals that are mild skin irritants may make a patient feel warm,” wrote Borrell et al., “but they will not produce any in vivo temperature rises or any of the physiological effects of heat.” The effect is just too superficial.
- Hinds T, McEwan I, Perkes J, et al. Effects of massage on limb and skin blood flow after quadriceps exercise. Med Sci Sports Exerc. 2004 Aug;36(8):1308–13. PubMed 15292737 ❐ “…any increase in SKBF is potentially diverting flow away from recovering muscle. Such a response would question the efficacy of massage as an aid to recovery in postexercise settings.”
- While in overview it may be all about “basic” hydrodynamics and fluid mechanics, the circulatory system is only analogous to plumbing, and it does things you can only explain with rheology, a branch of physics that deals with the flow of matter (in any state, but especially gasses, fluids, and soft solids).
- Wakim KG, et al. The effects of massage on the circulation in normal and paralyzed extremities. Archives of Physical Medicine & Rehabilitation. 1949;301:35–144. PubMed 18114696 ❐
- Hovind H, Nielsen SL. Effect of massage on blood flow in skeletal muscle. Scand J Rehabil Med. 1974;6:74–77. PubMed 4837058 ❐
- They also tested “pounding” or “hacking” massage (tapotement). This is not a widely used technique. It did increase the rate of blood flow through the muscle, “comparable to exercise.” Their opinion was that this is probably because it was highly stimulatory and was literally making the muscle contract! It was “exercise,” in other words. The more prolonged. But all this is rather academic, since tapotement accounts for only a tiny slice of what massage therapists do.
- Munk N, Symons B, Shang Y, Cheng R, Yu G. Noninvasively measuring the hemodynamic effects of massage on skeletal muscle: a novel hybrid near-infrared diffuse optical instrument. J Bodyw Mov Ther. 2012 Jan;16(1):22–8. PubMed 22196423 ❐
Munk et al. argue this persuasively, in the course of introducing a new experimental method — “a novel hybrid near-infrared diffuse optical instrument” — that has some impressive advantages. They write:
Previous MT studies investigating blood flow have actually used measures that do not directly assess the rBF [relative change in blood flow]. Rather, such studies make assessments of arterial width and blood velocity to extrapolate macro- hemodynamic properties or examine proxy assessments that are related to rBF such as oxygenation saturation levels or skin temperature. While meaningful data are gathered in studies which use these assessments, independently and directly measuring muscle rBF and oxygenation in MT studies is desirable to more fully understand the extent to which MT affects physiologic processes.
- Franklin NC, Ali MM, Robinson AT, Norkeviciute E, Phillips SA. Massage therapy restores peripheral vascular function after exertion. Arch Phys Med Rehabil. 2014 Jun;95(6):1127–34. PubMed 24583315 ❐ PainSci Bibliography 54263 ❐
- The researchers measured the ability of blood vessels to respond to changes (flow-mediated dilation as measured by ultrasound). The authors boil this idea down to “endothelial function,” and conclude that leg massage boosts it in the arms, both in people sore from a workout and not sore. Their tortuous, double-negative summary: “massage attenuates impairment of upper extremity endothelial function resulting from lower extremity EMI in sedentary young adults.”
- A low point is the obviously inadequate referencing to support “studies have demonstrated that MT enhances local circulation.” And repeatedly citing Crane’s notoriously over-interpreted study is another glaring concern. So I assume that these researchers were at great risk of finding what they went looking for.
- Zhang Q, Sun Z, Yue J. Massage therapy for preventing pressure ulcers. Cochrane Database Syst Rev. 2015 Jun;(6):CD010518. PubMed 26081072 ❐
- Ramos-González E, Moreno-Lorenzo C, Matarán-Peñarrocha GA, et al. Comparative study on the effectiveness of myofascial release manual therapy and physical therapy for venous insufficiency in postmenopausal women. Complement Ther Med. 2012 Oct;20(5):291–8. PubMed 22863643 ❐
- The authors tout only the statistical significance of their results, not their size, which almost always means a real effect that was too small to emphasize. And, sure enough, when I read the whole paper, it turned out that the effects measured were “technically positive” but modest at best, and in many cases trivial. A misleading overemphasis on statistical significance is a huge red flag in research, and the subject of much hand-wringing about the quality of modern research. See Statistical Significance Abuse.
- Sheng M, Yang J, Bao M, et al. The relationship between step count and all-cause mortality and cardiovascular events: A dose-response meta-analysis. J Sport Health Sci. 2021 Sep. PubMed 34547483 ❐ PainSci Bibliography 52202 ❐
This study shows that the health benefits of walking are both amazingly large and also “non-linear”: that is, you get a lot of benefit up front, a huge reduction in health hazards by the time you’ve hit 5K steps/day… at least double what you get out of the next 5K. The ten-thousand-steps “rule” is overkill for a lot of people.
Massage does not actually move a thrombus all the way from the calf to the lungs. Massage simply breaks it loose, and then it gets carried to the lung.
Venous clots stick to the walls of blood vessels, and are somewhat impeded by valves as well (where the vessel is a little narrowed). When physically disturbed, they can partly or entirely tear free. Once floating freely, there’s nothing to stop the chunks from being carried by the bloodstream until they get to the vessels too small to pass through, and the first place that happens is in the lungs.
Veins merge and enlarge as the blood moves towards the heart, like descending a tree. When it gets to the heart, it is given a big push into the lungs, where vessels rapidly start dividing and shrinking — and so the clot soon gets stuck, impeding or completely blocking circulation to all the vessels past that point.
This is a great example of why massage therapists actually need to study physiology.
- Warren SE. Pulmonary embolus originating below knee. Lancet. 1978 Jul;2(8083):272–3. PubMed 79075 ❐
Case report of an elderly woman who developed a lung embolus after her husband vigorously massaged her leg, which had a known deep vein thrombosis — a serious contraindication to massage which any competent massage therapist would certainly avoid. But not all of them…and not husbands as a general rule.
- Mikhail A, Reidy JF, Taylor PR, Scoble JE. Renal artery embolization after back massage in a patient with aortic occlusion. Nephrol Dial Transplant. 1997 Apr;12(4):797–8. PubMed 9141017 ❐
A case report: “massage” in the form of walking on the back (which is not as rare or necessarily as reckless as it sounds) dislodged a clot in the aorta at the site of a graft (aortobifemoral bypass graft). This is an unusual case (but not because of the massage), which is why they wrote it up: “It is controversial whether aortic occlusion can lead to retrograde thrombosis of the renal arteries.“ But it appeared to in this case, and that’s what the report is focused on. But the graft “occluded over a year before admission but the loin symptoms only appeared after the massage. We presume that in this case in the presence of normal renal arteries the physical trauma led to dislodgement of thrombus…”
- Jabr FI. Massive pulmonary emboli after legs massage. Am J Phys Med Rehabil. 2007 Aug;86(8):691. PubMed 17667202 ❐
This letter to the editor of The American Journal of Physical Medication & Rehabilitation describes a case of a 53-year-old woman with progressively worsening shortness of breath, which started after a “vigorous” massage of her calf muscles at a pedicure shop. She had “filling defects” in “several” lung arteries. She survived this: the emboli were successfully dissolved by anti-coagulants. But a close call for sure.
“Not only can [massage] dislodge an already established blood clot, but, as in this case, it can also predispose an individual to venous thrombosis and subsequent pulmonary embolism. … there is likely underreporting.”
- Lim DCG, Jayanthi HK, Money-Kyrle A, Ramrakha P. Massaging the outcome: an unusual presentation of pulmonary embolism. BMJ Case Rep. 2009;2009. PubMed 21687002 ❐ PainSci Bibliography 51824 ❐
This is a case study of a man who’d had deep vein thrombosis presumably caused by a long-haul flight (flex your ankles regularly on flights!). He was treated with anticoagulants for months, but the clot remained… until it was dislodged in a massage two years later. The massage was a “full-body” massage and included the legs, but no other details were noted. “The onset of dyspnoea soon after leg massage suggests that this was the likely cause of thrombus embolisation.” It does seem likely.
His only symptom was shortness of breath, which is impressive considering how serious the embolus was. It was a “worm-shaped right atrial embolus, most probably a femoral cast.” Meaning the embolus was basically the shape of the vessel where it had lived until it was dislodged, and wormed its way into a lung. Shudder.
- Behera C, Devassy S, Mridha AR, Chauhan M, Gupta SK. Leg massage by mother resulting in fatal pulmonary thromboembolism. Med Leg J. 2018 Sep;86(3):146–150. PubMed 28441907 ❐
This is case study of a young man who died because his mother gave him a leg massage after an ankle fracture. “Autopsy confirmed the cause of death as pulmonary thromboembolism due to deep vein thrombosis of the leg veins which was dislodged and travelled to his lungs consequent to the leg massage. The treating doctors did not warn the patient of the risk of developing pulmonary thromboembolism.”
- Sutham K, Na-Nan S, Paiboonsithiwong S, Chaksuwat P, Tongsong T. Leg massage during pregnancy with unrecognized deep vein thrombosis could be life threatening: a case report. BMC Pregnancy Childbirth. 2020 Apr;20(1):237. PubMed 32321459 ❐ PainSci Bibliography 51826 ❐
This is a case study of a pregnant woman who fell into a coma after a traditional Thai massage at a shopping center in Chiang Mai, Thailand. Her baby miscarried. The cause was a clot in her leg, which was dislodged and carried to her lungs, where it stuck, cutting off lung circulation.
About 10 minutes after her massage, the woman developed shortness of breath, became disoriented, convulsed, lost consciousness, and had a heart attack. She was initially resuscitated at the hospital, but remained comatose, and she remained unconscious for two months until the case report was written.
“Pregnant women are at a higher risk of undetected or subtle thromboembolism…” and “it is reasonable to conclude that the patient had undetected preexisting deep vein thrombosis, which was mechanically dislodged by the massage and travelled massively to both lungs, leading to a life threatening condition.”
I think the data we’d like to have on this simply doesn’t exist, and probably never will for all kinds of practical reasons. Very few contraindications have ever based on robust evidence. This is usually all we have got:
- Reasonable inference from known physiological and pathological premises, speculative answers to the question “what could possibly go wrong?”
- Case reports that confirm that the worst cases are at least POSSIBLE.
- The near certainty that most adverse events are under-reported.
- The precautionary principle.
And arguably that’s enough.
- Ingraham. 💩 Massage Therapists Say: A compilation of more than 50 examples of the bizarre nonsense spoken by massage therapists with delusions of medical knowledge. PainScience.com. 11683 words.
- UpToDate [Internet]. Goshima K. Overview of thoracic outlet syndromes; 2019 May 10 [cited 19 May 20]. PainSci Bibliography 52417 ❐
This is a speculative mechanism of thoracic outlet syndrome, and almost certainly not a common one, but it is plausible, and there are case studies of it. Qaja 2017 reported on “arterial TOS caused by hypertrophy of the anterior scalene muscle in a 65-year-old male” and Yürük 2016 reported on “a case of scalene muscle hypertrophy in long-term follow-up of diagnosis of cervical discopathy.” Digging into much older literature, an intriguing 1986 study (Machleder) of characteristics of the anterior scalene muscle found that it is “uniquely structured in fiber composition to sustain prolonged contraction” and in TOS patients it “demonstrates an extraordinary adaptive transformation and recruitment response in the type 1 fiber system reflecting chronic increased tone or motor neuron stimulation.” So the ASM may be a particularly hard-working muscle, for whatever reason, which is probably why it can get “hyooge” enough in some people to cause trouble.
Note that this phenomenon probably does not require dramatic growth of the scalenes. In many or most cases, it’s probably a (literal) collision of hypertrophy with anatomical abnormalities like cervical ribs. Some people probably just have less room for even minor scalene growth. But why would scalenes get beefy in the first place? Also, the regulation of muscle tone and contraction is one of the deepest rabbit holes in all of musculoskeletal medicine and pathology, and “unwanted contractions” are extremely common and not necessarily obvious. Examples abound, and I discuss many of them here: Cramps, Spasms, Tremors & Twitches. And then there’s just good ol’ fashioned bad habits: it’s completely speculative, but a common plausible source of scalene overdevelopment is dysfunctional breathing.
- Cramps and twitches are the tip of the iceberg — there are many major types of unwanted muscle contractions. There are also many myths about them: dehydration and magnesium deficiency don’t cause cramps, “stiffness” isn’t caused by “tight” muscles, and “back spasm” is just a way of saying how back pain feels, not how it works. While many common aches and pains feel crampy, no one knows if there is any such thing as a contraction that can cause pain without being otherwise seen or felt — but it is possible. See Cramps, Spasms, Tremors & Twitches: The biology and treatment of unwanted muscle contractions.
Trigger point massage has rarely been directly tested and never properly. There are only about a dozen studies worth knowing about, all have serious flaws, and most report only minor benefits at best (e.g. Hodgson 2006, Gulick 2011, Morikawa 2017.) The evidence may look a bit hopeful to a trigger point therapist, but science just hasn’t answered the question, and it is going to stay that way for quite a while.
The “expanded integrated hypothesis” was presented by Dommerholt, Gerwin, and Shah in 2004. It’s detailed and technical! When abridged and oversimplified, it closely resembles the integrated hypothesis (“a possible explanation”) put forward by Travell and Simons in the first edition of their famous textbook in 1981. The expanded integrated hypothesis basically says this:
Under some circumstances, muscular stresses can cause patches of poor circulation, which results in the pooling of noxious metabolic wastes and high acidity in small areas of the muscle. This is both directly uncomfortable, but also causes a section of the muscle to tighten up — a micro cramp — and perpetuate a vicious cycle. This predicament is often called an “energy crisis.” It constitutes a subtle lesion. TrPs research has largely been concerned with looking for evidence of a lesion like this.
- In practice, no one seems to think that brief pressure on a trigger point is an effective treatment. As a rule, sore spots do not stop being sore just because you press on them for a couple seconds. Which is interesting.
- For instance, imagine you vigorously exercise your quads for a few minutes and then, blood still racing, you push your thumb firmly into the top of your thigh. Guaranteed, despite all the blood rushing through the big vessels, you are easily stopping that blood from reaching the compressed tissues under your thumb. It is possible that trigger points are resistant to perfusion in the same way, even when there’s plenty of blood flowing. It’s also possible that this varies depending on the severity of the trigger point and other local anatomical factors. That is, exercise might help flush this trigger point just fine, but not that one.
- Stuiver MM, ten Tusscher MR, Agasi-Idenburg CS, et al. Conservative interventions for preventing clinically detectable upper-limb lymphoedema in patients who are at risk of developing lymphoedema after breast cancer therapy. Cochrane Database Syst Rev. 2015 Feb;(2):CD009765. PubMed 25677413 ❐ This is the most recent major scientific review available as of 2019, and it’s inconclusive: “Based on the current available evidence [10 trials], we cannot draw firm conclusions about the effectiveness of interventions containing MLD.”
- Huang TW, Tseng SH, Lin CC, et al. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomized controlled trials. World J Surg Oncol. 2013 Jan;11:15. PubMed 23347817 ❐ PainSci Bibliography 52885 ❐ “10 RCTs with 566 patients…”
- Pichonnaz C, Bassin JP, Lécureux E, et al. The effect of manual lymphatic drainage following total knee arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2016 Jan. PubMed 26829760 ❐
Testing manual lymphatic drainage is fairly easy and interesting, because it’s supposed to have such an objective, measurable effect on swelling. So how did five doses of MLD work on 30 patients who’d just had knee surgery (total knee arthroplasty)? Compared to 30 others who got a placebo. It didn’t work! No difference in swelling. MLD bombed this straightforward test. Alas.
- Ezzo J, Manheimer E, McNeely ML, et al. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev. 2015;5:CD003475. PubMed 25994425 ❐
This 2015 review of six studies of manual lymphatic drainage for breast cancer-related lymphedema is about as on-point as we can hope for if we want to know if MLD works. BCRL is the indication for which MLD is best known. Note that swelling reduction is by far the most important outcome measure.
And it’s a tepid mix. The conclusions aren’t wholly negative, but they are way less positive than they should be. There is some promising evidence here that suggests MLD probably helps some of these patients at least a little bit some of the time, but even that “needs to be confirmed.” And a couple studies showed some modest swelling reduction — but really not that much, or not even a statistically significant result.
But mostly the evidence is a classic example of damning with faint praise. There’s definitely a failure of MLD to demonstrate the kind of clear reductions in swelling we would like to see based on its reputation.
- Oliveira MMF, Gurgel MSC, Amorim BJ, et al. Long term effects of manual lymphatic drainage and active exercises on physical morbidities, lymphoscintigraphy parameters and lymphedema formation in patients operated due to breast cancer: A clinical trial. PLoS One. 2018;13(1):e0189176. PubMed 29304140 ❐ PainSci Bibliography 52424 ❐ “MLD is as safe and effective as active exercise in rehabilitation after breast cancer surgery.” But not more effective. And a massage technique really has to be better than exercise to be worth the expense of skilled help.
- Dreha-Kulaczewski S, Joseph AA, Merboldt KD, et al. Inspiration is the major regulator of human CSF flow. J Neurosci. 2015 Feb;35(6):2485–91. PubMed 25673843 ❐
There has never been any significant controversy over whether cerebrospinal fluid actually moves around (only whether or not it’s palpable or can be manipulated, with or without effect/benefit). This is an MRI study of how the fluid circulates, and it confidently concludes it’s pumped every time you take a breath in: “The present results unambiguously identify inspiration as the most important driving force for CSF flow in humans.”
This strongly suggests that the rhythm CST therapists claim to be able to feel is exactly in sync with respiration. Not so exotic! This is just one paper, and it isn’t necessarily the last word about the mechanism of CSF circulation, but it does strongly suggest that there is indeed a CSF circulation phenomenon to explain, and it’s powered in a straightforward way that probably can’t be significantly manipulated by any means other than holding your breath.
- Downey PA, Barbano T, Kapur-Wadhwa R, et al. Craniosacral therapy: the effects of cranial manipulation on intracranial pressure and cranial bone movement. J Orthop Sports Phys Ther. 2006 Nov;36(11):845–53. PubMed 17154138 ❐
This is a study of the effect of craniosacral therapy on rabbit skulls and their cerebrospinal fluid circulation. The researchers found that “low loads of force, similar to those used clinically when performing a craniosacral frontal lift technique, resulted in no significant changes in coronal suture movement or intracranial pressure in rabbits.”
If you can’t move rabbit skull bones or change their intracranial pressure, it’s safe to assume that you probably can’t do it to humans either — and without that mechanism in good working order, craniosacral therapy has no basis at all. The researchers concluded: “These results suggest that a different biological basis for craniosacral therapy should be explored.” But, of course, a “different biological basis” for craniosacral therapy has never even been suggested, let alone tested.
- Increased intracranial pressure gets serious with small increases in the fluid volume — only about a 100mL. There are well-described mechanisms that the body uses to try to compensate for increasing intracranial pressure: see the Monro-Kellie hypothesis. Expansion of the cranium is not one of the mechanisms that relieves pressure.
