Massage Therapy for Tension Headaches
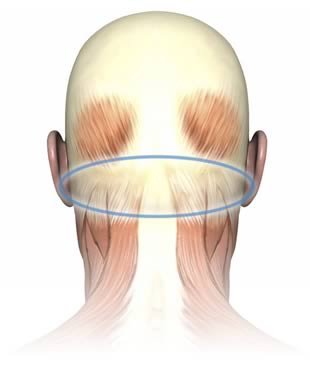
Perfect Spot No. 1, in the suboccipital muscles of the neck, under the back of the skull.
Trigger points (TrPs), or muscle “knots,” are a common cause of stubborn & strange aches & pains, and yet they are under-diagnosed. The 14 Perfect Spots (jump to list below) are trigger points that are common & yet fairly easy to self-treat with massage — the most satisfying & useful places to apply pressure to muscle. For tough cases, see the advanced trigger point therapy guide.
Under the back of the skull must be the single most pleasing and popular target for massage in the human body. No other patch of muscle gets such rave reviews. It has everything: deeply relaxing and satisfying sensations, and a dramatic therapeutic relevance to one of the most common of all human pains, the common tension headache. And no wonder: without these muscles, your head would fall off. They feel just as important as they are.
Along with lots of other neck muscles, the suboccipital group — usually just called “the suboccipitals” — work overtime to keep your head balanced on top of your spine. In particular, they initiate and control fine movements. This is no small task: if you’re a big person, your head may weigh as much as a 10-pin bowling ball, and it is resting on a foundation only about one third as wide. These muscles have to be workaholics.
The suboccipitals are also partly “antagonized” (balanced) by the jaw muscles. This is an odd arrangement. Generally speaking you’ve got one muscle or group of muscles that pulls one way, and then muscles on the other side of the joint that pull the other way. But the jaw muscles do not affect the spinal joints, and cannot directly work against/with the suboccipitals to balance the head. Nevertheless, they do: muscle studies have shown that the jaw muscles behave much like they would in a more normal push-pull relationship with the suboccipitals.[citation needed] They function together and dysfunction together. Both of these muscle groups routinely harbour trigger points that are linked to headaches and migraines,123 and I personally believe they cause a great many headaches — maybe more than any other cause.4
If I could have only one group of muscles to get massaged regularly, this is the one I’d choose. For example …
A simple success story: treating a tension headache with suboccipital massage
My cat once woke me up with a particularly insistent feed-me-now yowl. Normally I would have been irritated, but on that day she was doing me a favour, because my neck was in a crazy position and I was cooking up a violent headache. It was already spreading across the back of my skull like a toxic spill.
Sleeping is dangerous!
I can only assume it would have been even worse without my furry early warning system, but within an hour my headache was yowling more than the cat, who was by then fed and settled in the “cat sauna.” Late in her life, she became fond of sleeping in the bathroom with the heat lamp on — presumably it was therapeutic for her cranky ol’ body. I decided to follow her example and warmed the back of my head up with one of my big, thick and lovely Thermophore heating pads and then settled in for a dose of urgently needed massage for Perfect Spot No. 1. Then, using a Knobble massage tool, which is just perfect for this location, I applied some intense5 pressure to my suboccipital muscles. And then I followed that up with a good dose of mobilizations (simple neck circles).
The headache vanished. It’s hard to overstate the degree of success I enjoyed from this simple procedure. It was a severe headache, the kind that could easily ruin a whole day. Success was by no means guaranteed, and I feared the worst. But my self-treatment didn’t just take the edge off: the headache was terminated, quickly and completely. It was gone like it had never happened, and it did not come back. Such is the power of massaging the suboccipitals (sometimes).

The “Knobble II” by Trigger Point Products is a good shape for self-massage of the suboccipital area.
What does Perfect Spot No. 1 feel like?
In addition to generally producing the best quality of the “deep sweet ache” that most people crave from massage, trigger point referral into the head has a sedative feeling that can’t be beat. Just as trigger point referral elsewhere in the body often feels pleasantly “paralyzing,” creating a deadening or heavy feeling that usually spreads out and down like a heavy blanket, trigger point referral from the suboccipitals does this too — but into your head. With the right pressure, in the positive context of therapeutic massage, that sensation is deliciously soporific.
Many people report these positive sensations in this location, even those who aren’t otherwise especially “triggery,” and who may have the idea that massage is kind of pointless (a strange attitude, but it’s out there). When I worked as a massage therapist, I often observed that even quiet and unresponsive clients — taciturn, or just really zoned out — would clearly react to pressure in the suboccipitals. A client who hadn’t made a sound for fifty minutes would suddenly groan with relief and say, “Oh, that’s a good spot.” It’s that reaction that originally inspired this series of articles: it’s the prototypical “perfect spot” for massage.
Pain produced by trigger points in the suboccipitals is also often vague and “ghostly,” as Travell and Simons put it.6
How do you treat Perfect Spot No. 1?
The suboccipital group is easy to find. It lies just underneath the back of your skull, where it overhangs the neck, in a line from ear to ear. Each person’s personal version of Perfect Spot No. 1 will be found somewhere in that arc. While the entire group responds positively to pressure in most cases, there is some variation in quality from one location to another along the ridge.
The exact centre is the one spot where you might not get a positive reaction. There is a small hollow there, right at the top of the spine. To some people, pressure on this spot — which is not actually even muscular — will be sweet bliss. To others, while there is no actual danger, it feels too vulnerable, too “spine-y.” It’s a love-it-or-hate it spot, with roughly 75% of people loving it, 25% feeling uneasy with it. Note that some people can learn to love it, if they feel safe enough.
The rest of the region is all predictably pleasurable, but your partner’s favourite spot might be in the thinner roots of the tissue (higher on the back of the skull), or deeper into the muscle bellies (further under the ledge). They might prefer pressure on the thick bands of muscle exactly on either side of the centre, or they might prefer it way out on the sides, just behind the bump of bone under the ear.
To massage someone’s suboccipitals, have them lie down face up. Reach under the base of the skull and press upwards with your fingertips. Start slow, but most people will be able to tolerate strong pressure here. Beware: they won’t want you to stop.
How do you self-treat Perfect Spot No. 1?
It’s a bit tricky to effectively massage your own suboccipital muscles without a tool like the Knobble massage tool, which (as mentioned above) is just perfect for this particular location, but if you don’t have one (yet) it is also awfully nice to just lie down with this muscle group resting on a tennis ball. To some extent you can roll back and forth on that and get some satisfaction. A smaller, more accurate ball might work even better for you, or you could rest the centre point on the pointy end of a “Kong”-style dog toy (probably through a layer of fabric to soften it and keep the rubber from pulling your hair).
Another good therapeutic exercise for this muscle group is “neck circles,” and heat is usually more helpful than cold (although that always depends on your preferences).
Stretching is not all it’s cracked up to be, in general9 or as a treatment for trigger points,10 and for biomechanical reasons it’s tough to stretch the suboccipitals firmly: the chin can only drop so far.11 But you can elongate them, some people will get more out of it than others, and it is worth a try.
To stretch these tiny muscles as well as you can, slowly and respectfully pull your head downwards with your hands, but gently straighten your lower neck at the same time — that is, only tilt the skull forward (not your whole neck). Add a little bit of rotation to add some tension to one side or the other.
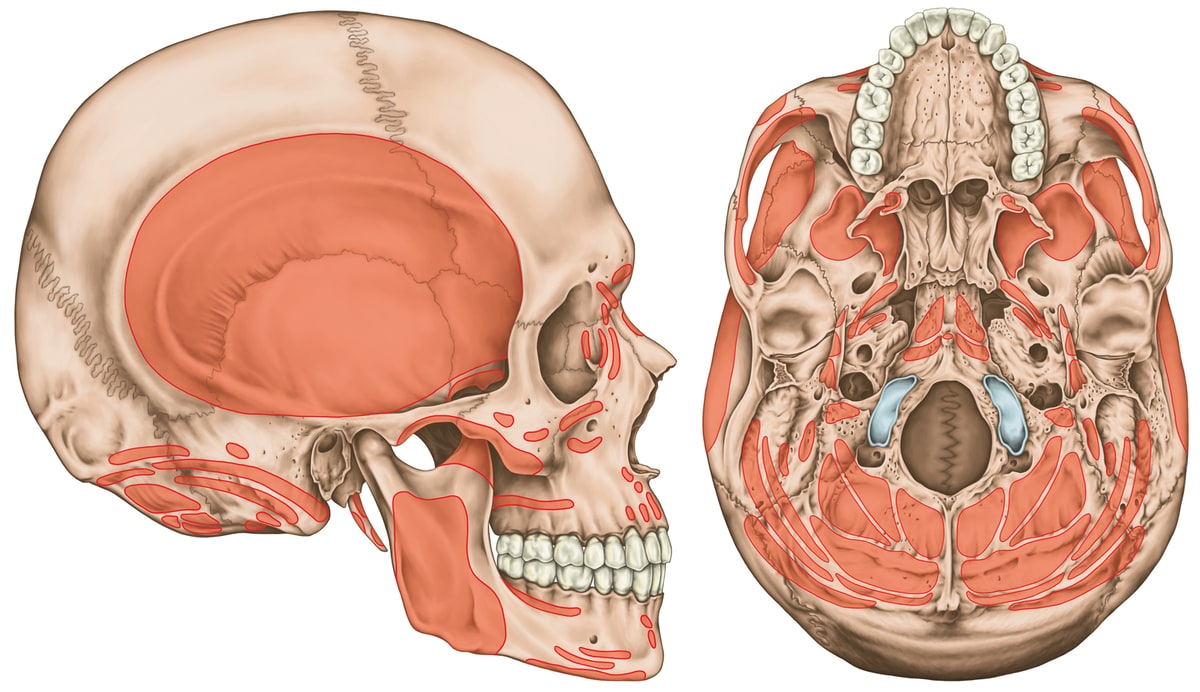
Muscle attachment areas of the skull… a lot of them, especially on the underside. Most of the muscles on the bottom of the skull are also neck muscles. Click to zoom.
Do you have a trigger point under your skull? Or is that just a cervical myodural bridge?
Brace yourself for humility! This is a fantastic example of how hard it is to be sure of anything in medicine.
Cervical myodural bridges are an inconsistent anatomical feature of the neck in some people. They are connections between the spinal cord wrapping (dura mater) and the muscles of the upper neck — basically some rogue gristle. Exactly what is connected and how tightly is debatable and is probably quite different from person to person, like all anatomy.12 The clinical implications are unclear, but they surely exist.13 CMBs probably explain why some people can flex their upper neck more comfortably than others, and it probably causes some headaches.
Obviously there’s not much to be done about a CMB, but you can at least get some sense of whether or not this might be a problem for you just by strongly flexing your upper neck (tuck your chin down firmly): if it’s uncomfortable, there’s a good chance you have pesky myodermal bridges!
Or just trigger points. Which are also sensitive to stretch.
It’s probably impossible to tell the difference between a neck that is sore because of trigger points and one that is sore because of a CMB. Some people might get suboccipital trigger points because of the irritation of a CMB always tugging on their spinal cord, so “all of the above” is definitely a possibility — and a fine example of how trigger points in this area could be just about invincible.
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the Internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Appendix A: Is trigger point therapy too good to be true?
Trigger point therapy isn’t too good to be true: it’s just ordinary good. It can probably relieve some pain cheaply and safely in many cases. Good bang for buck, and little risk. In the world of pain treatments, that’s a good mix.
But pain is difficult and complex, no treatment is perfect, and there is legitimate controversy about the science of trigger points. Their nature remains somewhat puzzling, and the classic image of a tightly “contracted patch” of muscle tissue may well be wrong. What we do know is that people hurt, and it can often be helped.
The Perfect Spots are based on a decade of my own clinical experience as a massage therapist, and years of extensive science journalism on the topic. Want to know more? This is the tip of the iceberg. I’ve written a whole book about it …
Not too good to be true.
Just ordinary good. Trigger point therapy isn’t a miracle cure, but it is a valuable life skill. Practically anyone can benefit at least a little, and many will experience significant relief from stubborn aches and pains. The first few sections are free.
Appendix B: Quick Reference Guide to the Perfect Spots
This index is also available on its own page.
1For headache, neck pain
Under the back of the skull must be the single most pleasing and popular target for massage in the human body. No other patch of muscle gets such rave reviews. It has everything: deeply relaxing and satisfying sensations, and a dramatic therapeutic relevance to one of the most common of all human pains, the common tension headache. And no wonder: without these muscles, your head would fall off. They feel just as important as they are. (Click/tap heading to read more.)
| for pain: almost anywhere in the head, face and neck, but especially the side of the head, behind the ear, the temples and forehead | muscle(s): suboccipital muscles (recti capitis posteriores major and minor, obliqui inferior and superior) |
2For low back pain
This Perfect Spot lives in the “thoracolumbar corner,” a nook between your lowest rib and your spine — right where the stability of the rib cage and thoracic vertebrae gives way to the relative instability of the lumbar spine. It consists of trigger points in the upper-central corner of the quadratus (square) lumborum muscle and in the thick column of muscle that braces the spine, the erector spinae. (Click/tap heading to read more.)
| for pain: anywhere in the low back, tailbone, lower buttock, abdomen, groin, side of the hip | muscle(s): quadratus lumborum, erector spinae |
3For shin splints
Perfect Spot No. 3 is in your shins — seemingly an unlikely place for muscle knots! But there is meat there, and if you’ve ever had shin splints then you know just how vulnerable that meat can be. Even if you’ve never suffered so painfully, your shins probably still suffer in silence — latent trigger points in the upper third of the shin that don’t cause symptoms, but are plenty sensitive if you press on them. (Click/tap heading to read more.)
| for pain: in the shin, top of the foot, and the big toe | muscle(s): tibialis anterior |
4For thoracic outlet syndrome, throat pain and tightness, chest pain
Deep within the Anatomical Bermuda Triangle, a triangular region on the side of the neck, is the cantankerous scalene muscle group. Massage therapists have vanished while working in this mysterious area, never to be seen again. The region and its muscles are complex and peculiar, and many lesser-trained massage therapists have low confidence working with them. (Click/tap heading to read more.)
| for pain: in the upper back (especially inner edge of the shoulder blade), neck, side of the face, upper chest, shoulder, arm, hand | muscle(s): scalenes (anterior, middle, posterior) |
5For carpal tunnel syndrome, tennis elbow
Just beyond your elbow, all the muscles on the back of your forearm converge into a single thick tendon, the common extensor tendon. At the point where the muscles converge, in the muscles that extend the wrist and fingers, lies one of the more inevitable trigger points in the body: Perfect Spot No. 5. It is constantly provoked both by computer usage today, and more often by the use of a pen in simpler times — and by the occasional tennis match, then and now, or maybe crocheting. (Click/tap heading to read more.)
| for pain: in the elbow, arm, wrist, and hand | muscle(s): extensor muscles of the forearm, mobile wad (brachioradialis, extensor carpi radialis longus and brevis), extensor digitorum, extensor carpi ulnaris |
6For gluteal and hip pain, sciatica, bursitis, low back pain
When you have back pain, buttock pain, hip pain, or leg pain, much or even all of your trouble may well be caused by trigger points in the obscure gluteus medius and minimus muscles, a pair of pizza-slice shaped muscles a little forward of your hip pocket. Other muscles in the region are usually involved as well, such as the gluteus maximus, piriformis, and the lumbar paraspinal muscles. However, the gluteus medius and minimus are a bit special: their contribution to pain in this area is particularly significant, and yet people who have buttock and leg pain rarely suspect that much of it is coming from muscle knots so high and far out on the side of the hip. (Click/tap heading to read more.)
| for pain: in the low back, hip, buttocks (especially immediately under the buttocks), side of the thigh, hamstrings | muscle(s): gluteus medius and minimus |
7For jaw pain, bruxism, headache
Your masseter muscle is your primary chewing muscle — not the only one, but the main one — and it covers the sides of the jaw just behind the cheeks. It’s also the main muscle that clenches your jaw and grinds your teeth, unfortunately, and it’s one of the most common locations for trigger points in the human body. It is probably an accomplice in most cases of bruxism (that’s Latin for “grinding your teeth”) and temporomandibular joint syndrome (jaw joint pain), plus other unexplained painful problems in the area. (Click/tap heading to read more.)
| for pain: in the side of the face, jaw, teeth (rarely) | muscle(s): masseter |
8For runner’s knee
A lot of quadriceps aching, stiffness and fatigue emanates from an epicentre of “knotted” muscle in the lower third of the thigh, in the vastus lateralis, a huge muscle — one of your biggest — that dominates the lateral part of the leg. Stretching it is effectively impossible, but massage is an option: although often shockingly sensitive, Perfect Spot No. 8 can also be quite satisfying. It also often complicates or contributes to other problems in the area, especially runner’s knee (iliotibial band syndrome). (Click/tap heading to read more.)
| for pain: in the lower half of the thigh, knee | muscle(s): quadriceps (vastus lateralis, vastus intermedius, vastus medialis, rectus femoris) |
9For chest pain & tightness
The “pecs” are popular: of 700+ muscles, the pectoralis major is one of just a dozen or so that most people can name and point to. It also harbours one of the most commonly-encountered and significant trigger points in the human body, and can produce pain much like a heart attack in both quality and intensity. (Click/tap heading to read more.)
| for pain: anywhere in the chest, upper arm | muscle(s): pectoralis major |
10For plantar fasciitis
The tenth of the Perfect Spots is one of the most popular of the lot, and right under your feet — literally. It lies in the center of the arch muscles of the foot. This is one of the Perfect Spots that everyone knows about. No massage is complete without a foot massage! (Click/tap heading to read more.)
| for pain: in the bottom of the foot | muscle(s): arch muscles |
11For upper back pain
This “spot” is too large to really be called a “spot” — it’s more of an area. The thick columns of muscle beside the spine are often littered with muscle knots from top to bottom. Nevertheless, there is one section of the group where massage is particularly appreciated: from the thick muscle at the base of the neck, down through the region between the shoulder blades, tapering off around their lower tips. There is no doubt that this part of a back massage feels even better than the rest — even the low back, despite its own quite perfect spots, cannot compete. (Click/tap heading to read more.)
| for pain: anywhere in the upper back, mainly between the shoulder blades | muscle(s): erector spinae muscle group |
12For low back and gluteal pain, sciatica
At the top of the buttocks lies a Perfect Spot for massage: a sneaky but trouble-making brute of a trigger point that commonly forms in the roots of the gluteus maximus muscle. It’s below the lowest part of the low back, but it often feels like low back pain. This is the kind of spot that the Perfect Spots series is all about: not only does it tend to produce a profound, sweet ache when massaged, but the extent of the pain that spreads out around it is almost always a surprise. It feels like a key to much more than expected. (Click/tap heading to read more.)
| for pain: in the lower back, buttocks, hip, hamstrings | muscle(s): gluteus maximus |
13For low back pain, sciatica
Some of the Perfect Spots are perfect because they are “surprising” — it’s delightful to find a place to massage that feels highly relevant your pain in an unexpected location. Others are perfect because they are exactly where you expect them to be — and what a relief it is to be able to treat them. Perfect Spot No. 13 is perhaps the ultimate, the quintessential example of a trigger point that is usually “right where I thought the problem was”: in the “pit” of the low back, at the bottom of the thick columns of back muscle beside the spine. (Click/tap heading to read more.)
| for pain: in the low back, buttocks, hamstrings | muscle(s): erector spinae muscle group at L5 |
14For shoulder pain
I avoided adding Spot 14 to this series for many years, because it’s a bit tricky to find. But precision is not required: although there is one specific spot that’s especially good, nearly anywhere under the ridge of bone on the shoulder blade is worthwhile, and often a surprising key to pain and stiffness everywhere else in the shoulder, especially all the way around on the other side, facing forward. (Click/tap heading to read more.)
| for pain: any part of the shoulder, and upper arm | muscle(s): infraspinatus, teres minor |
What’s new in this article?
2023 — Science updated. Added a citation about the relationship between trigger points and headaches, and updated related footnotes a bit.
2017 — Added new section, “Do you have a trigger point under your skull? Or is that just a cervical myodural bridge?” Added more detail about stretching. Plus several other minor improvements.
2005 — Publication.
Notes
- Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache. 2006 Mar;46(3):454–60. PubMed 16618263 ❐
- Do TP, Heldarskard GF, Kolding LT, Hvedstrup J, Schytz HW. Myofascial trigger points in migraine and tension-type headache. J Headache Pain. 2018 Sep;19(1):84. PubMed 30203398 ❐
There is good evidence that people who get headaches — both migraine and “tension” — also have a lot of trigger points in the musculature of the head and neck. Unfortunately, we still have no idea which came first, the chicken or the egg: headaches might be causing trigger points, or trigger points might be causing headache. There is evidence pointing each direction, but all of it is all low quality and inconclusive. However, the simple correlation is relatively unambiguous: they are linked, we know that much at least.
Although the authors of this review are likely somewhat biased — “believers” in the clinical significance of trigger points, and interpreting the evidence through that lens — their conclusions are appropriately cautious, acknowledging the limitations of the evidence.
- Calandre EP, Hidalgo J, Garcia-Leiva JM, Rico-Villademoros F, Delgado-Rodriguez A. Myofascial trigger points in cluster headache patients: a case series. Head & Face Medicine. 2008 Dec 30;4(32):32. PubMed 19116034 ❐ PainSci Bibliography 55349 ❐
Although this research was “preliminary and uncontrolled” and is not powerful enough to prove anything, its results were certainly noteworthy — the sort of results that can inspire more research, hopefully. All of 12 patients with chronic cluster headaches (a kind of severe primary headache, nicknamed “suicide headaches”) had myofascial trigger points, and treating them (with injection) produced “significant improvement in 7 of the 8 chronic cluster patients.” The authors speculate that trigger points are not the cause of cluster headaches, but a nasty complicating factor: “chronic pain or repeated acute pain sensitize muscular nociceptors creating active trigger points which, in turn, contribute to potentiate headache pain. This kind of vicious cycle explains why the number of active trigger points has been found to be higher in patients with chronic primary headaches than in healthy subjects or in patients experiencing less frequent headache attacks.”
My claim here that trigger points are not only a cause but the most common cause of headaches is mostly based on my own clinical observations. There is no good quality data to back that up at this time. The evidence I just cited cannot support the “most” part. But I am placing my bet: in time, I think the evidence will show that the relationship is in fact a strong, bottom-up causal relationship.
- I already know from lots of experience that strong massage pressure is safe and appropriate for me — please be cautious with strong pressure!
- Travell J, Simons D, Simons L. Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Lippincott, Williams & Wilkins; 1999.
- Sun F, Yuan QL, Zhang YG. Large Buttocks Hematoma Caused by Deep Tissue Massage Therapy. Pain Med. 2015 Jul;16(7):1445–7. PubMed 26176792 ❐ PainSci Bibliography 51701 ❐
- Note that superficial bruising from massage is common and different from rupturing "arteries and veins." Many techniques can cause significant breakage of the capillaries and other very small vessels just under the skin. It’s unsightly and intimidating, and of course some of the techniques may *also* cause larger and deeper contusions, but most of it is relatively harmless subcutaneous bruising. I don’t approve of techniques that do this, but it’s definitely not in the same league as breaking larger vessels.
- Stretching is not a pillar of fitness: it doesn't warm you up, enhance peformance, or prevent or treat soreness, injury, or any kind of chronic pain. But it can actually backfire! It can boost flexibility, for whatever it’s worth (not much). For more information, see Quite a Stretch: Stretching science has shown that this extremely popular form of exercise has almost no measurable benefits.
- Although stretching is the first thing everyone tries to do for stiff, sore muscle, in practice results are erratic and usually minor at best. If trigger points are “mini cramps,” stretching might help some of them — or it might be more like trying to untie knots in a bungie cord by pulling on them. See the stretching article for more on this interesting stretching sub-topic.
- Neck flexion is stopped by the chin hitting the chest, sharply limiting suboccipital stretch in most people. Although mildly stretchable in some people, it’s impossible for others, and an awkward and limited stretch for most. Many other muscles are similarly awkward to stretch, some of them just more or less impossible — see The Unstretchables.
- Palomeque-Del-Cerro L, Arráez-Aybar LA, Rodríguez-Blanco C, et al. A Systematic Review of the Soft-Tissue Connections Between Neck Muscles and Dura Mater: The Myodural Bridge. Spine (Phila Pa 1976). 2017 Jan;42(1):49–54. PubMed 27116115 ❐
This review of 26 studies found “strong evidence” and concluded that it “proved” that there are connections between some suboccipital muscles and the dura mater, while there is “limited evidence” and “controversy” about others. They conclude: “There is a continuity of soft tissue between the cervical musculature and the cervical dura mater.”
- Enix DE, Scali F, Pontell ME. The cervical myodural bridge, a review of literature and clinical implications. J Can Chiropr Assoc. 2014 Jun;58(2):184–92. PubMed 24932022 ❐ PainSci Bibliography 53727 ❐