Patellofemoral Pain Diagnosis with Bone Scan
If you have anterior knee pain, should you bother x-ray, MRI, CT scan, or bone scan?
“Curiously, neither the widespread use of arthroscopy nor the advent of new diagnostic tests such as CT scanning and magnetic resonance imaging have cast much light on the enigma of patellofemoral pain,”1 and MRI in particular is not of much use diagnostically except to eliminate some diagnoses that can usually be made pretty easily without MRI.2
MRI is surprisingly uninformative or misleading in musculoskeletal medicine; it particularly is notorious for that with back pain. Many causes of body pain have little to do with visible anatomical oddities or degeneration and injury, even when those are present — the real story is often metabolic, neurological, and microscopic, not “mechanical.”
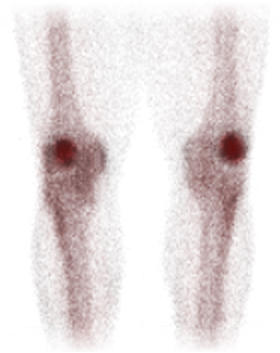
Fortunately, X-rays and bone scans for patellofemoral pain are a different matter — they are worthwhile, and potentially quite interesting. It’s been suggested since Dye et al. in 1986 that increased metabolic activity can be imaged using bone scans.3 An initial study confirmed that this was true for PFPS Hejgaard et al.4 Any patient with stubborn, severe and/or atypical patellofemoral pain syndrome should consider pursuing these diagnostic options. There are significant diagnoses that simply cannot be made without them.
In more recent science, that was the main finding of Näslund et al.’s 2006 study of diagnosing PFPS. In 75 patients that were clinically indistinguishable from each, they found 17 cases of disease — quite a lot.5 Quite a few more (29) had “hot,” metabolically active kneecaps,6 where bone is busily remodelling. In a similar study the year before, the same researchers found 48 hot knees out of 109 cases.7
All patients and 48 healthy subjects without any knee pain were then interviewed and examined by a surgeon and a physical therapist. They could not diagnose the pathologies without the scans! All patients with pain tested roughly the same, and their symptoms were indistinguishable.
In 2003, Lorberboym et al. investigated the PFPS-detection power of a SPECT scintigram — a bone scan with a better camera, basically.8 They compared SPECT bone scanning to arthroscopy — literally looking at the inside of the knee with surgery — and it performed very well, with some caveats.9
All of this gives good support to Dr. Dye’s theory of metabolic distress — a major theme in my patellofemoral pain book.
How do you scan your bones?
Bone scanning is a nuclear imaging technique: a radioactive tracer is injected and then detected, showing up where blood flow is the greatest — which indicates metabolic activity. They are absolutely fascinating. My wife had a bone scan after she was seriously wounded in a car accident in 2010. We watched the tracer on a monitor, spreading through her body in real time — incredible. She lit up like a Christmas tree: more glowing fractures and cracks that we didn’t know about yet.
How to get a bone scan for knee pain
X-rays are commonplace, of course, but bone scans are a bit of a big deal, expensive and not always easy to get, especially SPECT. Your physician or surgeon may be puzzled by a request for a bone scan. In this case, you should respectfully refer them to a scientific paper: perhaps Dr. Dye’s 2005 paper about patellofemoral pain syndrome, or perhaps Näslund et al.’s paper, which has a well-written overview.
The case for getting a bone scan if you have patellofemoral pain
It shouldn’t be your first stop, and none of the more radioactive imaging techniques should be for any minor musculoskeletal problem. However, if your case proves to be stubborn — as patellofemoral pain often can be — it can quickly become a priority.
Any condition which results in a change in the metabolism of the bone will result in a change in the appearance of the bone scan. Lesions like fractures, infections, tumors, and arthritis can be recognized on a bone scan long before they can be seen with plain radiographs. More importantly, the technique has been proven to be useful in confirming a diagnosis of patellofemoral pain syndrome, and in helping to isolate the distressed tissues — exactly which bone is stressed.
If a bone scan clears you of disease, and shows that you’ve got a hot kneecap, then you have a much clearer idea of what you’re dealing with.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
This article is a free chapter from PainScience.com’s huge patellofemoral pain syndrome (PFPS) tutorial, one of 103 chapters in all. There are also several other excerpts and articles on the site about patellofemoral pain and related topics:
- Massage Therapy for Your Quads — Perfect Spot No. 8, another one for runners, the distal vastus lateralis of the quadriceps group
- The Causes of Runner's Knee Are Rarely Obvious — The science shows that you usually can’t blame IT band pain or patellofemoral pain on the structural quirks that seem like “obvious” problems
- Is Knee Pain More Common in Women? — The relationship between sex and knee pain, especially runner’s knee (IT band syndrome, patellofemoral pain)
- What Can a Runner With Knee Pain Do at the Gym? — Some training options and considerations for runners (and others) with overuse injuries of the knee
- Does Cartilage Regeneration Work? — A review of knee cartilage “patching” with autologous chondrocyte implantation (ACI)
- Diagnosing Runner’s Knee — It usually starts with lateral knee pain during and after runs, but there are two major types
- Should You Get A Lube Job for Your Arthritic Knee? — Reviewing the science of injecting artificial synovial fluid, especially for patellofemoral pain
- Does Hip Strengthening Work for IT Band Syndrome? — The popular “weak hips” theory is itself weak
- Patellofemoral Pain & the Vastus Medialis Myth — Can just one quarter of the quadriceps be the key to anterior knee pain?
- Patellofemoral Tracking Syndrome — The beating heart of the conventional wisdom about patellofemoral pain is mostly nonsense
- Knee Debridement is a Completely Ineffective Procedure — Evidence that arthroscopic knee surgery for osteoarthritis is about as useful as a Nerf hammer
- Is Running on Pavement Risky? — Hard-surface running might be a risk factor for running injuries like patellofemoral pain, IT band syndrome, shin splints, and plantar fasciitis
Notes
- Insall JN. The patella. Springer Verlag; 1995.
- Quibble: MRI can be helpful in confirming tendinosis. However, it’s fairly rare for tendinosis to be confused with PFPS in the first place.
- Dye SF, Boll DA. Radionuclide imaging of the patellofemoral joint in young adults with anterior knee pain. Orthop Clin North Am. 1986;17(2):249–262.
- Hejgaard N, Diemer H. Bone scan in the patellofemoral pain syndrome. Int Orthop. 1987;11(1):29–33. PubMed 3557753 ❐
- They didn’t say which diseases. 15 cases of pathology were identified by X-ray, and many or all of these were probably minor, and simply results in a new and more specific diagnosis than PFPS. 2 cases were identified by bone scan … which can identify tumors.
- What exactly does that mean? It means that the bone is busily adapting to stress, making and/or breaking down bone tissue. Näslund et al.: “Bone metabolism and bone remodelling can be evaluated by specific bone seeking radionuclides in a scintigraphic measurement. A positive bone scintigraphy indicates an increase in bone metabolism, but the method cannot determine whether the final result will be a net loss or a net gain in bone. A pathophysiologically increased bone scintigraphy indicates an aetiological relationship between the area with increased bone metabolism and the patient’s symptoms.”
- Näslund JE, Odenbring S, Näslund UB, Lundeberg T. Diffusely increased bone scintigraphic uptake in patellofemoral pain syndrome. Br J Sports Med. 2005;39:162–165. PubMed 15728696 ❐ PainSci Bibliography 56679 ❐
- Lorberboym M, Ami DB, Zin D, Nikolov G, Adar E. Incremental diagnostic value of 99mTc methylene diphosphonate bone SPECT in patients with patellofemoral pain disorders. Nucl Med Commun. 2003 Apr;24(4):403–10. PubMed 12673169 ❐
- SPECT was super sensitive — 100%, actually — in detecting patellofemoral abnormalities! Alas, it was only 64% specific, meaning it didn’t just detect PFPS, but other conditions like patellar arthritis. Hopefully the future will bring techniques with more specificity for PFPS specifically.