Vagus nerve hype and hope (Member Post)
It’s hard to avoid the vagus nerve these days.
“The vagus” has become the One Nerve to Rule Them All, the wellspring of wellness when working, the master of malaise when “dysfunctional” or “misfiring” — behaviour it is accused of constantly. Unlike more ordinary nerves, the special vagus can apparently cause trouble without being in trouble: immaculate neuropathy.
Stimulating and “resetting” the vagus are now considered treatments in themselves, but for years the vagus has been the “explanation” for why many other treatments are effective. This is especially true of mindfulness/meditation empire, which claims to have firm scientific foundations, but most importantly the power of vagal tone and heart rate variability — almost unavoidable sub-topics.
Dig a little deeper into mindfulness science, and sketchy “polyvagal theory” — or even sketchier interpretations of it — will almost certainly make an appearance as well.
There are now many products and treatment methods that promise to induce deep relaxation, at the least, or deliver more profound healing effects — all by stimulating or “resetting” the vagus nerve in various ways.
Most of them are ripe bullshit, of course.
For instance, one advertiser claims that “there is a way to heal trauma-induced chronic pain” by “working directly with the vagus nerve” with “topic experts in vagal toning.” And what’s the problem with the vagus nerve, according to this advertiser? It’s “likely weak.” 🙄 🤣
It would be easy to make fun of these claims. But this post will fight nonsense with actual information instead of snark. (Mostly.)
Vagus nerve basics
A dozen big nerves emerge from the base of the brain and brain stem — the cranial nerves. The vagus is the tenth of these numbered nerves, cranial Nerve “X” (they are traditionally numbered with Roman numerals). It descends through the neck, where it’s bundled with the carotid artery and jugular vein, and then into the torso, branching heavily to connect to major nerve clusters, the lungs, the heart, and the stomach and guts. Although “the” vagus nerve is routinely referred to as though we have only the one, they are a functional unit and a nearly symmetrical pair, only taking different paths in the chest, the left one veering towards the back.
As a celebrity nerve, every interesting fact about the vagus nerve gets trotted out to support vagal hype. For instance, the vagus nerve is big even for a cranial nerve, and so we often see the claim that it is “longest nerve in the human body” — which is not quite right. It probably is the longest autonomic nerve, but the sciatic nerve is almost certainly the longest nerve of any kind.2
The vagus nerves are the crown jewels of the autonomic nervous system, the subsystem that’s dedicated to controlling physiology. The vagus nerve used to be known as the “pneumogastric” nerve: the lung-gut nerve! But it does more: it generally regulates most major physiology, tuning things like heart and respiratory rate, blood pressure, and digestion.
What is vagal tone?
Vagal “tone” is a real thing, but also a vague thing, hard to even define. It refers to the sum total of the vagus nerve’s effects. It’s almost (but not quite) synonymous with your “mood.” It is the physiology of your mood. More technically, your vagal tone is where you’re at on the spectrum of sympathetic to parasympathetic activation. It can refer to your current status, or to your average status over time, all other things being equal. A person suffering from chronic stress and anxiety could be said to have “poor vagal tone.” But this isn’t particularly different from just saying that they are stressed and anxious!
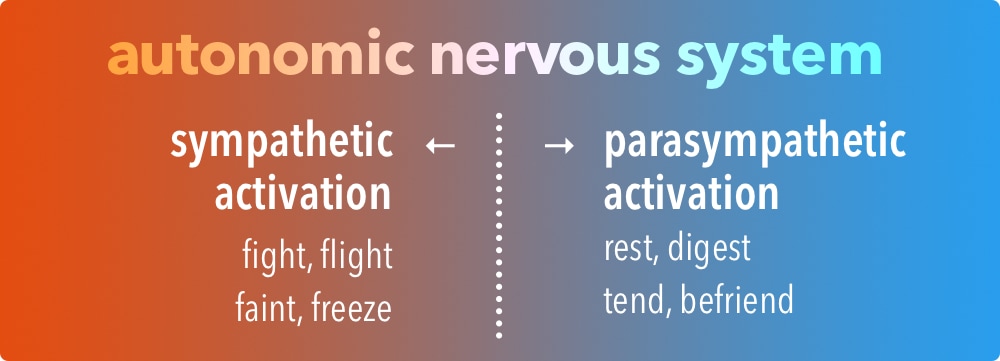
Vagal "tone" is your average position on the spectrum of autonomic nervous system activation, from the "hot" end to the "cool" end. Someone with high vagal tone would be, on average, further towards the "rest and digest" end than someone with low vagal tone (all other things being equal).
Vagal tone cannot be measured directly in any meaningful way. Instead, it is imprecisely represented by some surprisingly basic numbers. How basic? Try the heart rate. Slower? Higher vagal tone. Faster? Lower vagal tone! It is also represented by some additional heart beat nuances, like differences in the speed of the heart during inhalation and exhalation, the famous “heart rate variability” (HRV) number. There’s a whole section about that below. For now, you just need to know that it’s squishy and actually unimportant, and it’s not clear that HRV is even a useful metric in research.
There’s a reason your doctor does not tell you about your “vagal tone” along with your blood pressure: because it means almost nothing.
The rest of this post is for members only, another few minutes of reading. JOIN NOW (for USD $5/month or $50/year) to reveal another 1400 words, about five minutes of reading, or eight if you really want to learn it. I do one of these members-only posts once in a while, and membership unlocks the archives, as well as about twenty members-only sections scattered around the site, plus audio-only versions. See more information about membership. ❐ Topics beyond the paywall:
- Can you “reset the vagus nerve”? (Spoiler alert: no, duh, but it’s fun to explain why)
- Carotid sinus massage and the vagal manoeuvres: screwing around with your vagus nerve
- Polyvagal theory
- Neuromodulation and vagus nerve stimulation

Pause, cancel, or switch plans at any time. Payment data handled safely by Stripe.com. More about security & privacy. PainScience.com is a small publisher in Vancouver, Canada, since 2001. 🇨🇦
The salamander’s domain is for people who are serious about this subject matter. If you are serious — mostly professionals, of course, but many keen patients also sign-up — please support this kind of user-friendly, science-centric journalism.
Can you “reset the vagus nerve”?

My “check vagus” light has been nagging me for weeks now! Always keep the vagus nerve inflated to about 25-30 PSI, and periodically check for signs of uneven wear. An annual defragging wouldn’t hurt either.
The fantasy is that the vagus nerve is the “master nerve” of stress physiology, and therefore stress can be relieved by taming it with a relatively simple procedure: the reset. The underlying assumption is that the vagus nerve gets chronically dysfunctional, sending the wrong signals, causing or sustaining all kinds of physiological dysfunction. But that’s like blaming the steering wheel for bad driving.
The reset metaphor is absurd. The vagus nerve and its role in physiology may be legitimately interesting, but it’s not some kind of magic switch for stress. It is critical for stimulating “rest and digest mode,” yes, but that does not mean that you can induce relaxation or relieve stress just by stimulating the nerve, any more than you can walk by tickling your sciatic nerve. What the vagus nerve gets up to remains mostly up to the brain. The vagus nerve is just the messenger: it implements a bunch of physiological policy, and you can’t generally trick it into doing something else.
You can trick it in some minor and specific ways: see “vagal manoeuvres” below.
And it’s possible that stimulating the vagus nerve electrically has some physiological effects and benefits, some of which are relevant to pain.
But you cannot “reboot” the vagus nerve like its a computer, forcing it to do a generally better job of regulating your physiology. That is just simplistic wishful thinking.
Carotid sinus massage and the vagal manoeuvres: screwing around with your vagus nerve
True story: when your heart is misbehaving in a specific way (supraventricular tachycardia), a doctor may be able to slow it down by rubbing the carotid sinus or “bulb” in your neck. Pressure on this spot is just about the closest thing there is to a real “Vulcan neck pinch,” because it can cause dramatic drops in blood pressure.3 This is not especially complicated, and in fact it’s even possible to trigger it accidentally (if you have carotid sinus hypersensitivity), causing big swings in heart rate and/or blood pressure. Some experts have even speculated that this might even explain some heart attacks. 😮
The closely related “vagal manoeuvres” all trigger vagal nerve activity via reflex effects:
- The “diving reflex” is triggered by holding your breath and getting your face cold and wet — a biological feature we’ve probably inherited from marine ancestors. So that’s nifty, and I can imagine some practical utility.4 This is probably the origin of the widespread notion that cold water immersion is a way to “reset” the vagus nerve (which is wrong in several ways).
- Being upside down does it too. And so does compressing the abdomen. And coughing. These three might all be powered by the same mechanism (and could also be related to diving, in fact).
- What else? Triggering the gag reflex! I’m not joking. I have no clever evolutionary explanation for this one.
These are genuine neurological hacks — and they are the seeds of truth which have been fertilized with a lot of bullshit to grow profitable vagus “reset” or “toning” claims.
The vagus nerve and polyvagal theory
Worship of the vagus nerve as the key to the power of the mind over the body appears to be almost entirely thanks to Stephen Porges and “polyvagal theory.” Without PVT, no yoga teachers or massage therapists would be talking about “resetting the vagus nerve” today. PVT and its implications overlap a fair amount with the science — or pseudoscience — of heart-rate variability science.5
Polyvagal theory is a controversial and perpetually-unvalidated hypothesis cooked up by neuroscientist Stephen Porges in the 90s. The idea was that neurological control of the viscera via the autonomic nervous system — via the vagus nerve — has a third major division in addition to the familiar sympathetic and parasympathetic: the “social engagement system,” which either boosts or suppresses our ability to engage socially.6
That idea isn’t widely embraced by modern neuroscientists or evolutionary biologists, but it has become a darling of alternative medicine and psychologists. And Porges is still out there writing papers and books and “promoting” PVT … not so much as a psychotherapeutic modality in itself, but as a rationale for a variety of interventions (like meditation).
PVT didn’t start out as pseudoscience, but I think that it has evolved into it — because the evidence doesn’t support it,7 and because it has been thoroughly exploited and corrupted by cranks and hacks.
Neuromodulation and Vagus Nerve Stimulation (mostly with electricity)
Central stimulation is stimulation of the spinal cord or brain with electricity. It’s possible to do this non-invasively, but probably not possible to do it well. To get it right, you’ve got to get right in there with an actual implant: more invasive, profound, and dangerous, but also more impressive results for more serious problems like Parkinson’s diseases, major depression, and severe chronic pain.9
The vagus nerve is essentially just an extension of the brain, so vagus nerve stimulation (VNS) is closely related in spirit. But it’s a more superficial structure, so it’s potentially easier to “reach.” And its functionality is related to all kinds of things that might be of clinical interest. So it’s not surprising that it’s a hot topic.
Nor is it surprising that “more study is needed.” Not a single benefit has come anywhere close to being “proven.” Meanwhile, of course, there are VNS clinics and VNS gadgets and VNS programs springing up everywhere.
What might VNS do?
- It’s possible that vagus nerve stimulation can attenuate inflammation in rheumatoid arthritis patients — an extremely interesting possibility, but also far from an established effect.10 If true, it would probably have important implications for other inflammatory and painful conditions. But there is virtually no clinical trial evidence to look at so far.
- VNS might suppress seizures, too. But no one’s quite sure about that yet.11
- Depression might yield to VNS.12 But good luck citing anything definitive on that score.
Never forget that “a promising treatment is the larval stage of a disappointing one.”13 That said, some types of central and deeper forms of neuromodulation are plausible, interesting, and legitimate. I think this topic is well worth watching over the next decade. We just have to be cautious to filter out the hype. But when isn’t that the case? Hype infects every hopeful idea in medicine!
The vagus nerve more than most, however.
↑ MEMBERS-ONLY AREA ↑
Notes
- Apple is the most profitable gadget maker in history, and has repeatedly leveraged the power of X in their branding and marketing (most notably with “macOS X” and “iPhone X”). Why? Because they know that people respond to the letter X! In the same weird way that words that with ‘k’ in them are useful for comedians. Most people aren’t even aware that the vagus nerve is the X’th cranial nerve X! But they don’t need to be, because ‘V’ for vagus also has marketing potency. I honestly don’t think it’s a coincidence that the Xth cranial nerve with a widely known V-name is held in such regard. If it was the fourth cranial nerve and named the “George” nerve, there’s no way it would be so celebrated. Humans are weird.
Anatomical “facts” like this are often very difficult to confirm in my experience. You need a directly relevant anatomy paper, but most papers about the anatomy are focused on that anatomy, and not on fun-fact comparisons with other anatomy. The “longest nerve” claim is just obviously wrong, and probably a predictable, bias-serving exaggeration. The sciatic nerve is basically the length of the thigh. The vagus nerve length is a bit ambiguous, because it branches so heavily, but the “trunk” persists at least to the top of the abdomen... and that distance could only be longer than the thigh in quite an oddly shaped human. For instance, I am very short, and I have quite short legs relative to my torso. So if any reasonably normal human has a shorter thigh length than brain-stomach, it might be me — and yet my thigh is a little longer. Most people will clearly have a longer thigh.
The carotid sinus is a widening of the carotid artery where the common carotid artery splits into the internal and external carotid, at the level of the Adam’s apple and basically the same place you take a carotid pulse. The “carotid crotch” is richly innervated with nerves that detect blood pressure (baroreceptors). We can squish the bulb to trigger a reflex that changes heart behaviour and drops blood pressure! In practice it’s messier, but that’s basically the idea.
This reflex is not actually mediated by the vagus nerve, and technically has nothing directly to do with the vagus nerve, and so carotid sinus massage is not actually a “vagal manoeuvre” — but it is functionally so similar that they are usually grouped together. They are as similar as canoes and kayaks. The vagus nerve even has its own baroreflex, but it’s triggered by a nerve cluster in your aorta — so good luck massaging that one without surgery.
But the vagus nerve is immediately adjacent to the carotid sinus — it’s right there — and so it’s also possible that direct physical stimulation of the vagus nerve during carotid sinus massage is relevant, and could even account for how carotid sinus massage doesn’t always have completely predictable effects. But that’s pure speculation on my part.
Imagine you’re fighting off a panic attack. Your physiology is spinning out of control, powered by adrenalin, and it’s useless telling it to calm down. But you know that there’s a hard-wired reflex that will slow your heart down a little: just splash cold water on your face and hold your breath slightly longer than you can comfortably manage, enough to trigger the diving reflex. Your neurology “knows” that this situations means that slowing your heart rate is an extremely high priority.
Could work. 😜
- HRV is ideal for pseudoscience: a noisy system that generates plenty of data that can be interpreted essentially any way you want, about as objectively meaningful as a Rorschach test. And this is exactly how PVT exploits it.
- Porges SW. Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology. 1995 Jul;32(4):301–18. PubMed 7652107 ❐
This is a simple translation of the abstract: no editorializing here, just putting it into relatively plain English.
The vagus nerve regulates the guts, including and especially the heart. Its emerges from two distinct areas of the brain, the nucleus ambiguus and dorsal motor nucleus. These regions are both connected to the heart via the vagus nerve, but (hypothesis) the NA fibres are responsible for coordinating heart rate with respiration (respiratory sinus arrhythmia). “Divergent shifts in RSA and heart rate are explained by the independent actions” of these areas. Polyvagal theory emphasizes the evolution of this system and proposes that mammals (as opposed to reptiles) have an area of the brain stem (including NA) devoted to attention, motion, emotion, and communication, which can sometimes be at odds with signalling from the dorsal motor nucleus, and this could explain clinical disorders like sudden infant death syndrome and asthma. So polyvagal theory is basically the idea that the viscera are regulated (via the vagus nerve) by two different parts of the brain stem that don’t always play well together.
Thirty years later, it remains a hypothesis — and a somewhat obscure one, barely discussed by experts today. Its major premises are not well supported by any direct evidence.
- Ben Cormack, Peter Stilwell, Sabrina Coninx, Jo Gibson. The biopsychosocial model is lost in translation: from misrepresentation to an enactive modernization. Physiotherapy Theory and Practice. 2022:1–16. PubMed 35645164 ❐ PainSci Bibliography 52047 ❐
This thoughtful paper argues that Engel’s biopsychosocial model (“an important framework for musculoskeletal research and practice”) has been misapplied in 3 ways:
- biomedicalization — just paying lip service to humanism & holism, but still being really rather biomedical
- fragmentation — tendency to perceive patients' complaints as this or that (e.g. bio or psycho or social), instead of this AND that (it’s always all of the above)
- neuromania — it’s ALL about the 🧠!
Result? “Suboptimal musculoskeletal care,” in the opinion of the authors.
I explore this paper and topic in much more detail in BPS-ing badly! How the biopsychosocial model fails pain patients.
- This approach has roots in electroconvulsive therapy — “electroshock” therapy back in the day — but the modern era of electrical therapy began when deep brain stimulation was introduced in 1987, and it’s been steadily improving since then, mostly thanks to better surgical techniques for implants.
- Koopman FA, Chavan SS, Miljko S, et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc Natl Acad Sci U S A. 2016 Jul;113(29):8284–9. PubMed 27382171 ❐ PainSci Bibliography 53670 ❐
Vagus nerve stimulation sure sounds great (maybe a little too great): stimulate your vagus nerve with an implant, et voila, less systemic inflammation. There’s broad biological plausibility here, but almost no evidence — this idea hinges only on the results of this one study so far. Koopman et al. tested it on humans and reported that “these results establish that vagus nerve stimulation targeting the inflammatory reflex modulates TNF production and reduces inflammation in humans.”
Established, eh? Not without replication! That’s overconfident for sure — this needs replication before celebration.
All kinds of data hijinks could be hiding in a study this technical. My main concern is the use of the word “significantly” in the abstract, without any details (effect size in particular). All too often that wording, without clarification, means there was a statistically significant but clinically trivial result. With many treatment trials I can go digging for the effect size to confirm, but not here, the reading is too difficult for me to form any meaningful impression without spending an hour, and even then it might not be clear. And even if the paper does indicate a clinically meaningful result it’s still got “too good to be true” written all over it and may well prove to be difficult to reproduce.
But it’s a genuinely interesting topic, I think.
- Lampros M, Vlachos N, Zigouris A, Voulgaris S, Alexiou GA. Transcutaneous Vagus Nerve Stimulation (t-VNS) and epilepsy: A systematic review of the literature. Seizure. 2021 Oct;91:40–48. PubMed 34090145 ❐
- Conway CR, Kumar A, Xiong W, et al. Chronic Vagus Nerve Stimulation Significantly Improves Quality of Life in Treatment-Resistant Major Depression. J Clin Psychiatry. 2018 08;79(5). PubMed 30152645 ❐
- Bastian H. "They would say that, wouldn't they?" A reader's guide to author and sponsor biases in clinical research. J R Soc Med. 2006 Dec;99(12):611–4. PubMed 17139062 ❐ PainSci Bibliography 51373 ❐
