Neurodynamic Stretching
Stretching and stimulating nerves to treat neuropathy… hopefully
The goal of neurodynamic stretching is to stretch and stimulate nerve tissue specifically — not muscles.
Neurodynamic stretching is a technical type of stretching, usually provided by a professional, designed to treat neuropathy by stretching nerves. It is a bit obscure, and the science is thin, but it’s an interesting idea that’s been around for a long time. It may also partly explain why common, simple stretching feels so darn good.
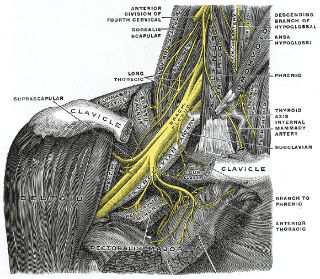
Some pain is caused by physical interference with nerves — neuropathies like carpal tunnel syndrome or sciatica.1 Neural mobilization or neurodynamics is a loose collection of experimental stretching and positioning treatments for neuropathy based on the idea that “unhappy” nerve tissue can be helped with the stimulation of stretch.
But not just any movement! Only quite specific movements need apply. If you really know your stuff, you can move in a way that emphasizes effects on nerves rather than muscles and tendons. “Stretching” isn’t really a good term, an oversimplification to get us started without too much jargon. More specifically, it may be possible to slide nerves in their sheathes (neural gliding or sliding or, the goofiest term, neural flossing)… or just pulling on the whole thing (neural tensioning). Some of the movements superficially look like conventional stretching, but neural sliding and tensioning are also possible without anything that looks like stretching at all.
Overlap with stretching
To the extent that neurodynamics can involve some stretch-like movements — some versions are “stretchier” than others — it is good example of a specialized type of stretching that might have genuine benefits for some patients. Indeed, perhaps more than stretching in general, which is not only hugely overrated as a therapeutic tool or pillar of fitness,3 but also conspicuously lacking in supposedly “advanced” methods that are proven to be superior to just doing whatever feels nice.
If neurodynamics is effective, it would be an impressive partial vindication of therapeutic stretching. Spoiler alert: no one actually knows if it works, because…
Neurodynamics: barely studied
There is plenty of science that’s relevant to the underlying principles, but not clinical trials of its application. Nerves have been studied plenty, but not the efficacy of nerve stretching as a treatment — not nearly enough anyway.
Neural mobilization is a tough thing to test — technical, hard to standardize, rotten with confounding factors. The science is so threadbare that it barely registers. I’ll just cite two small reviews,45 both doomed attempts to pull a useful signal out of a little bit of noise, a small collection of mediocre trials. This is an annoyingly common problem at the fringes of musculoskeletal medicine, which is surprisingly primitive in general.6
They both seem like good news, but don’t read the fine print if you want to remain hopeful: as always in this field, there’s nothing but minor temporary benefits reported, and even that may just be the result of biased and sloppy research. 🙄 Wishful thinking is a helluva drug — even for researchers (or perhaps especially for researchers).
So neurodynamics is not a scientifically validated therapy. But it hasn’t actually been kicked to the curb yet either. It remains plausible and interesting, and no advanced discussion of stretching for pain would be complete without it.
Meet the wire-pipes
“Wiring” seems like the obvious metaphor for nerves, but “plumbing” is surprisingly apt as well. Nerves may not be as much like pipes as blood vessels, but they are actually more like pipes than wires when it comes to how they work. They are like fancy plumbing doing an impressive imitation of an electrical system.
All nerves are tubes filled with fluid. Although the fluid doesn’t flow, it is wet, which is necessary for all the messy chemistry that allows nerves to play with electricity (just like in batteries). Their clever simulation of a flowing “current” is achieved by ions zipping back and forth across the membrane (action potentials), not by flowing along the length of the nerve (think of a stadium “wave”).
No pipe or wire works like that, of course. These physiology metaphors always fall apart when you start looking too closely.
Nested pipes
The chemistry of nerve impulses is sensitive to any interference with the integrity of that membrane. Wires can be kinked like a garden hose with no loss of functionality, but not nerves. Inflammation and other biochemical sources can also mess with nerve function (e.g. several poisons).
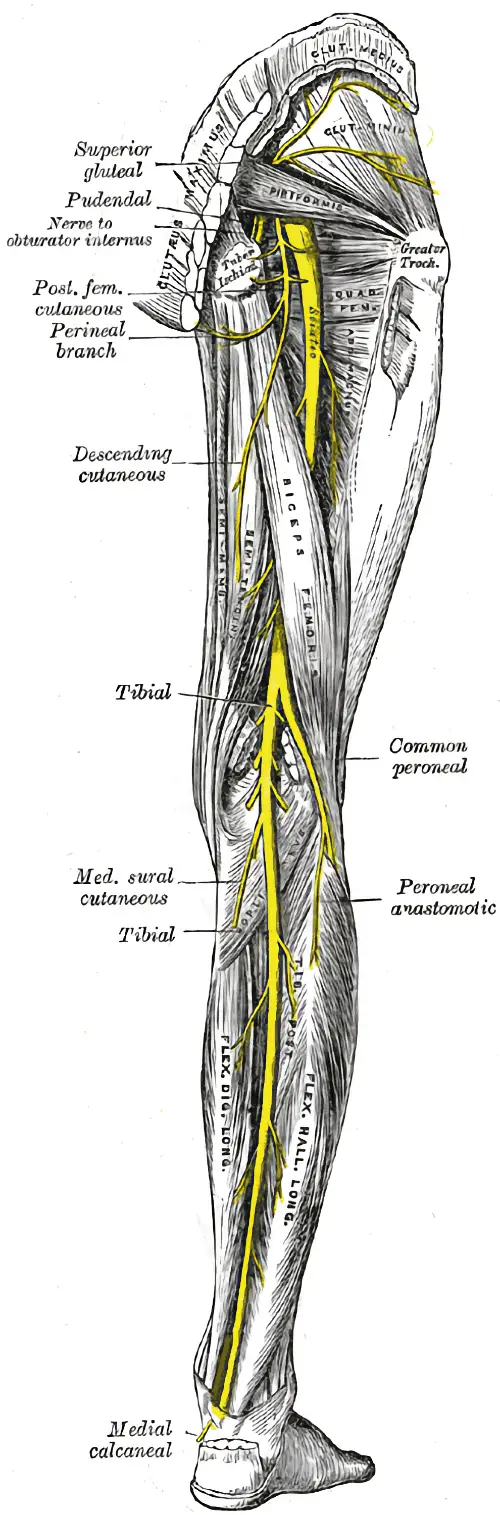
Many causes of neuropathy are simple, just straight up pinching. But there are more subtle paths to neuropathy — like not gliding smoothly in their sheaths. Most nerves have a wrapping, but it doesn’t function like the insulation on a wire. Nerves need their own specialized fluid environment for optimal function, so they are a fluid-fluid tube inside another fluid-filled tube. Nested pipes! Exactly like the way the brain and spinal cord are also packed in fluid, just smaller. The whole nervous system is packed in fluid like this, from nerves as thick as your thumb to nerves so tiny they make hairs look like tree trunks.
They are all packed in fluid, and they are all free to slide in those fluid-filled channels to some degree.
Unless they aren’t.
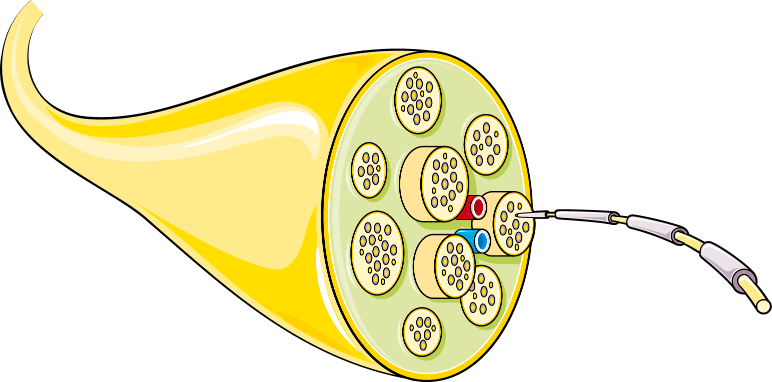
Larger peripheral nerves consist of bundles of nerve fibres, bundled into larger bundles along with blood vessels — nested “pipes.”
Tunnel syndromes and neural tension: the consequences of nerve snags (from the reasonably certain to the highly speculative)
Sometimes, due to pathological processes and physical predicaments, nerves get pressed against and stuck to the walls of their tubes, like microscopic velcro. This predicament is usually called “neural tension” or a “tunnel syndrome.” You don’t want this happening to your nerves any more than your cat wants tape on its paws. It affects their function.7
There are several infamous and obvious “tunnel syndromes,” most notably carpal tunnel syndrome.8 A more obscure example — yet still fairly common — is Baxter’s neuritis, or tarsal tunnel syndrome.
Subtler tunnel syndromes
For every pathologically blatant tunnel syndrome, there could be many subtler ones, and these might cause a lot of milder neuropathy. This is unconfirmed, but not especially controversial. This scenario is usually called “neural tension” rather than a “tunnel syndrome.”
But what if we ventured even further out onto this limb? What if the most subtle neural stuckness can cause symptoms that would never actually be diagnosed as neuropathy? Just vague aches and twinges and discomfort? Some experts have proposed that these little micro nerve entrapments are actually the specific cause of the “trigger point” phenomenon — humanity’s plague of unexplained sore spots.9
An interesting hypothesis, but that’s all it is so far. It’s completely unclear whether these subtler scenarios happen at all, or to what degree, or whether it is possible to treat them.
Free the nerves! One goal of neural mobilization is to break adhesions
“It’s trapped, I say! Trapped!”
You may have guessed it from the setup: one major goal of neural gliding is to free the nerves, by stretching in such a way that they actually pull free of their putative adhesions and entrapments. This sounds traumatic, but it could be so microscopic that we don’t feel a thing as it happens, or only the normal discomfort of a strong stretch.
Anything that feels like a stretch is undoubtedly causing many, many nerves to slide in their sheaths to some degree, and maybe this is a reason why stretch feels good/healthy: because it breaks up lots of little neural adhesions. Which may or may not exist. And probably not much more than miscellaneous physical activity, and maybe not all, but still, it might be why people like stretching. Just keeping those wire-pipes slip-sliding around nicely!
Neural gliding as a formal therapeutic method is more focused: specific stretches based on detailed anatomical knowledge required to apply maximal tension to specific nerves. There are professionals who have devoted a great deal of energy to learning how to tug on many different nerves.
Heck of a thing, really. Imagine pursuing so much specialized knowledge about a largely unvalidated approach to solving a problem that may or may not exist. Welcome to musculoskeletal medicine!
Story time: self-serve neurodynamic stretching to the rescue?
Articles with anecdotes get 78.2% better engagement.10 So here’s a wee yarn about a reader’s success treating sciatica by, quite possibly, pulling her sciatic nerve free from the wall of its sheath. As you do.
After years of minor chronic back pain, she had a rapid escalation into full-blown sciatica over the course of a couple days. Her “instinct” was to stretch — maybe wise, maybe lucky. Experimenting rather freely, she deliberately tried to stretch in the way that most clearly exacerbated her symptoms — which takes some guts, and obviously isn’t necessarily safe, and the kind of thing I wouldn’t dare to actually recommend. Several minutes into her experimentation, she experienced a painful surge … and then complete and lasting relief.
“The impression of a ripping sensation was so vivid that I felt like I almost heard it, even though it probably wasn’t audible. The pain was 90% gone instantly. All the throbbing leg pain that had been driving me nuts and keeping me awake for 2 days was just gone. There was still a little deep burn left, but I think it was like how the site of a bad sliver is still tender after the sliver is out. I slept fine, and by the next morning it there simply wasn’t any pain left.”
And here’s another one, from a physical therapist:
“My wife — 8 weeks post partum, history of low-moderate level aching back pain with excess activity — tweaked her back a bit picking up a child. Then she began having a gnawing, aching pain in the right glute, anterior hip, and upper thigh. It was intense enough that she decided to take ibuprofen (which she never does) and I started to try to figure out what was going on. She reported more pain with sitting, so I had her try a set of prone press ups to see if we would get any symptom modulation. No dice and she said flexing and left lateral flexion felt better. Next we tried a straight leg raise test to see if that could provoke the symptoms. She actually reported relief, so I had her do 15 supine sciatic tensioners. After completing she had a total relief of symptoms and it has not returned since.”
Both of these stories might be about actually physically liberating some nerve tissue from an anatomical trap of some kind. But we can only speculate! And if such things happen at all, it’s probably fairly rare. But no one really knows.
Now check out this 143-year-old example of another story like this…
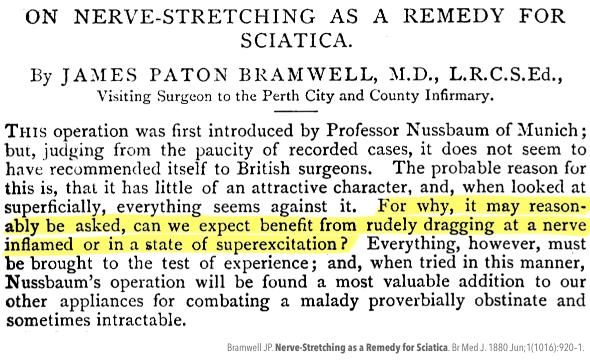
Why indeed would one want to “drag at" an inflamed nerve? In 1880, Dr. Bramwell reckoned it was to break up adhesions.11 And he might have been right. But it also might be simpler than that. (Hat tip to Tom Jesson for this old citation.)
A humbler goal: maybe it’s just nerve exercise?
Those stories support the adhesion-busting idea … but that’s more or less the only support it’s got. And although neural gliding often does have the goal of breaking adhesions between nerves and their sheathes, not everyone thinks that’s the point. There is another reason to mobilize, stretch, tension, slide, glide, or floss nerves…
Rather than targetting icky sticky nasty adhesions, maybe the main point of neural tensioning is just to pull on nerves, without optimizing for “glide” of the nerve within a sheath to break adhesions. That is, some stretches pull on both sheath and nerve more equally.
I am not aware of any specific rationale for this, other than the basic idea that it’s basically just a way of stimulating/exercising them, which is in turn is widely regarded a Good Thing.
And maybe it’s good enough. Indeed, some professionals think that’s the only defensible goal of any kind of nerve stretching. Not everyone agrees that the purpose of neurodynamic stretching is to rip free nerves from possibly imaginary adhesions or entrapments (which might not be clinically significant even if they do exist).
Pretty much everything in physiology seems to thrive on just-right levels of stimulation. “Motion is lotion” and “exercise is the closest thing we have to a miracle cure” and so on. And stagnancy of nerve tissue itself — not just the tissues they are connected to — might actually be a factor in neuropathy, an exaggerated version of how uncomfortable we get when stuck in one position for too long.
Do nerves need their very own exercise?
This justification for nerve stretching is probably on firmer ground than “it’s the entrapment, stupid,” but it’s still far from a slam dunk. I don’t think anyone doubts that stimulation is good for nerves in some sense, but … do we have to specifically stretch nerves to achieve it? Is it clinically important to do so?
It could be. Not everything in biology functions or heals well solely with the stimulation of normal activity!12
On the other hand, a great many medical interventions and “crutches” that supposedly facilitate healing have turned out to be surprisingly useless or even harmful.13 What actually assists the body is not obvious. Rigorous study is the only way we’re ever really going to know if specifically stretching nerves is helpful — as opposed to, say, something else specific like stretching blood vessels, or something general like just doing some calisthenics.
The rigorous study has not been done, of course. Until it is done, the value of nerve stretching cannot possibly be anything better than an educated guess.
Nerve tension and stretch tolerance
Hitting the natural and pathological limits of how far nerves can be pulled is one of the things that determines how intense a stretch feels. We may think we’ve stretched as far as we can not because we’ve hit the mechanical limit of the extensibility of our tissues, but because we’ve moved a nerve as far as it can be moved in its sheath. Nerve stretch may be what causes discomfort when you’re deep in a hard stretch, and it might be why some stretches are more unpleasant to hold than others.
This is particularly important because our “tolerance” for stretch is probably the main thing that changes when we increase our flexibility — not the actual physical properties of our tissues. I explore this concept in great detail in my stretching article.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
What’s new in this article?
Although first published as an independent article on Jun 8, 2021, the content was originally created a bit earlier as a chapter for my stretching article on April 25. I decided it warranted a page of its own.
2023 — Added a lovely anecdote about a dramatic success with neurodynamic stretching.
2022 — New section: “A humbler goal: maybe it’s just nerve exercise?”
2021 — Miscellaneous editing and revision after publication as an independent article. Added artwork and pull quotes.
2021 — Publication.
Notes
- Well-known neuropathies include sciatica, carpal tunnel syndrome, and shingles. Banging your “funny bone” (the ulnar nerve) is technically a brief, trivial neuropathy. In musculoskeletal medicine (the focus of PainScience.com), we are mostly concerned with relatively simple neuropathies caused by impingement and trauma, and not so much by disease… but not necessarily. Pain is complex, and sometimes it is caused by neuropathy with a complex pathological backstory.
Blood flow restriction training, AKA compression band training or “flossing” is basically exercising muscles while choking off their blood supply with big elastic bands. The idea is that this helps build strength and muscle mass. It’s not clear how exactly. BFRT is a more focussed and extreme version of the older idea of compression garments for performance and rehab — mostly tight leggings and sleeves — which have a long history of vague claims, and evidence of only trivial physiological and sensory effects (Weakley).
- Stretching is not a pillar of fitness: it isn’t a good warm-up, and it doesn’t enhance peformance, and it won’t prevent or treat soreness or injury. But it can cause injuries, and it can impair performance (slightly). It will boost flexibility, for whatever that is worth — which is surprisingly little (even for most athletes). Many major muscles are just mechanically impossible to stretch in the first place. Stretch might help some kinds of pain, like muscle pain, but stretching is clearly not of much help to most chronic pain patients. There is no “advanced” stretching method that overcomes any of these limitations, but you can spend a lot of money on books and courses and certifications — stretching is surprisingly big, snake oil. But, yes, it does feel good. See Quite a Stretch: Stretching science has shown that this extremely popular form of exercise has almost no measurable benefits.
- Basson A, Olivier B, Ellis R, et al. The Effectiveness of Neural Mobilization for Neuro-Musculoskeletal Conditions: A Systematic Review and Meta-Analysis. J Orthop Sports Phys Ther. 2017 Jul:1–76. PubMed 28704626 ❐
The level of evidence for neural mobilization is “largely unknown” according to this review of forty studies (only seventeen with a low risk of bias, and with lots of variety in methods throughout). The results were mixed, and NM notably failed for relatively straightforward peripheral neuropathies like carpal tunnel syndrome — if NM is good for anything, it should be good for that, at least.
On the bright side, according to the paper, the data “reveals benefits of NM for back and neck pain,” but these are complex conditions and notoriously multifactorial, so I remain pessimistic in the absence of more and better data. As the authors understate: “Due to the limited evidence and varying methodological quality, conclusions may change over time.” I’d say it’s so likely that “conclusions may change” that the word “conclusion” isn’t really useful here.
- Peacock M, Douglas S, Nair P. Neural mobilization in low back and radicular pain: a systematic review. J Man Manip Ther. 2022 May:1–9. PubMed 35583521 ❐
A review of eight studies of neural mobilization for back pain specifically, six of them with results in the “technically positive” category, but nothing impressive. As with Basson in 2017, there’s barely enough data to review, let alone for a rigorous meta-analysis. This is good fuel for wishful thinking for now, and that’s about it.
- We can put a man on the moon, but we can’t treat chronic pain. The science and treatment of pain and injury was neglected for decades while medicine had bigger fish to fry, and it remains a backwater to this day. The seemingly simpler “mechanical” problems of injury and rehab have proven to be surprisingly weird and messy. Oversimplification and quackery still dominate the field. For more information, see A Historical Perspective On Aches ‘n’ Pains: Why is healthcare for chronic pain and injury so bad?
- The membrane of the nerve itself is no longer floating freely, so ions can no longer rush in and out of that section of membrane quite so well. The result: pain, numbness, tingling.
- The tunnel term mainly refers to glaring cases of nerves that have gotten pinched in some of the larger, more obvious nerve sheathes, like the carpal tunnel. The tunnel can get narrowed by various mechanisms, like swelling, and adhesions may also form (basically getting pinched and then also stuck).
- Quintner JL, Bove GM, Cohen ML. A critical evaluation of the trigger point phenomenon. Rheumatology (Oxford). 2015 Mar;54(3):392–9. PubMed 25477053 ❐ Quintner et al. have hypothesized that “irritated peripheral nerve trunks” are “a rich source” of pain, and may be the true cause of trigger points, rather than the more conventional idea that they are “micro cramps.”
- Source? My arse. And 20 years publishing experience in this business, common sense, and knowledge of human nature. We like stories a lot, even though we all know we’re not supposed to take them too seriously.
- Bramwell JP. Nerve-Stretching as a Remedy for Sciatica. Br Med J. 1880 Jun;1(1016):920–1. PubMed 20749539 ❐ PainSci Bibliography 51427 ❐
- A simple example: deliberately washing wounds is dramatically better at preventing infection than just letting nature take its course. Simple mechanical flushing can be extremely powerful.
- Orthopedic surgery is one of the most relevant and obvious categories, and in that category nothing is more startlingly counterintuitive than the example of unnecessary tendon repair. It seems like ruptured tendons cannot possibly heal without being surgically anchored. But biology was healing tendon ruptures long before surgeons came along! Achilles tendon re-rupture is only slightly less likely with surgery… and with more complications (Ochen).