What Happened To My Barber?
Either atlantoaxial instability or vertebrobasilar insufficiency causes severe dizziness and vomiting after massage therapy, with lessons for health care consumers

My barber has this story: he had an incredibly severe negative reaction to the first and last massage he’d ever had. Not in my office — I was a Registered Massage Therapist at the time — but from another RMT. He had sought help for chronic tension headaches and neck pain (which often go together). The massage felt good at the time. But he was so dizzy afterwards that he couldn’t stand or drive properly, and he vomited several times when he arrived home.
“Uh oh,” I said. “What did the therapist tell you?”
“He told me that massage had released a lot of toxins into my bloodstream. Is that true?”
Absolutely not true! Repeat after me, everyone: severe dizziness and repeated vomiting is not a normal reaction to massage therapy!1 Nor is it a normal reaction to any other kind of physical therapy. Anyone experiencing such symptoms should consult a physician promptly.
This is a disturbing case. It’s troubling to think that a professional with the same training I had could tell a client something so irresponsible — in theory, we know better. My barber has been walking around with a potentially lethal misconception of what is going on in his neck! It is a classic example of how alternative health care professionals with inadequate training may put their patients at risk by failing to recognize ominous signs and symptoms, or take them seriously.
What really happened to my barber? Probably atlantoaxial instability
Beauty Parlour Syndrome is a stroke caused by sustained neck extension while hair-washing, probably usually caused by vertebrobasilar insufficiency, but there are other possibilities.2 I’d never heard of beauty parlour syndrome when I first wrote this article, and I didn’t encounter it for several more years. What happened to my barber was the same thing in principle — just in the hands of a massage therapist instead of a hair-dresser.
My barber didn’t know about beauty parlour syndrome either, apparently.
The details of his case are a good match with compression of the brain stem, as could be caused by a loose upper spine (known as atlantoaxial instability, AAI for the rest of this article, or more descriptively called upper cervical instability). It’s also possible that he had a problem with impairment of blood flow to the brain, which I’ll discuss in the next section.
AAI is a loss of the integrity of the joint between the top vertebrae of the cervical spine — called the “atlas” — and the one beneath it, the “axis.” AAI may be caused by an old injury to the neck. If this is what my barber has, when he moves his neck in a certain way, a small, finger-like projection of bone from his second cervical vertebrae could poke him in the brain stem, with consequences ranging from unpleasant to lethal.
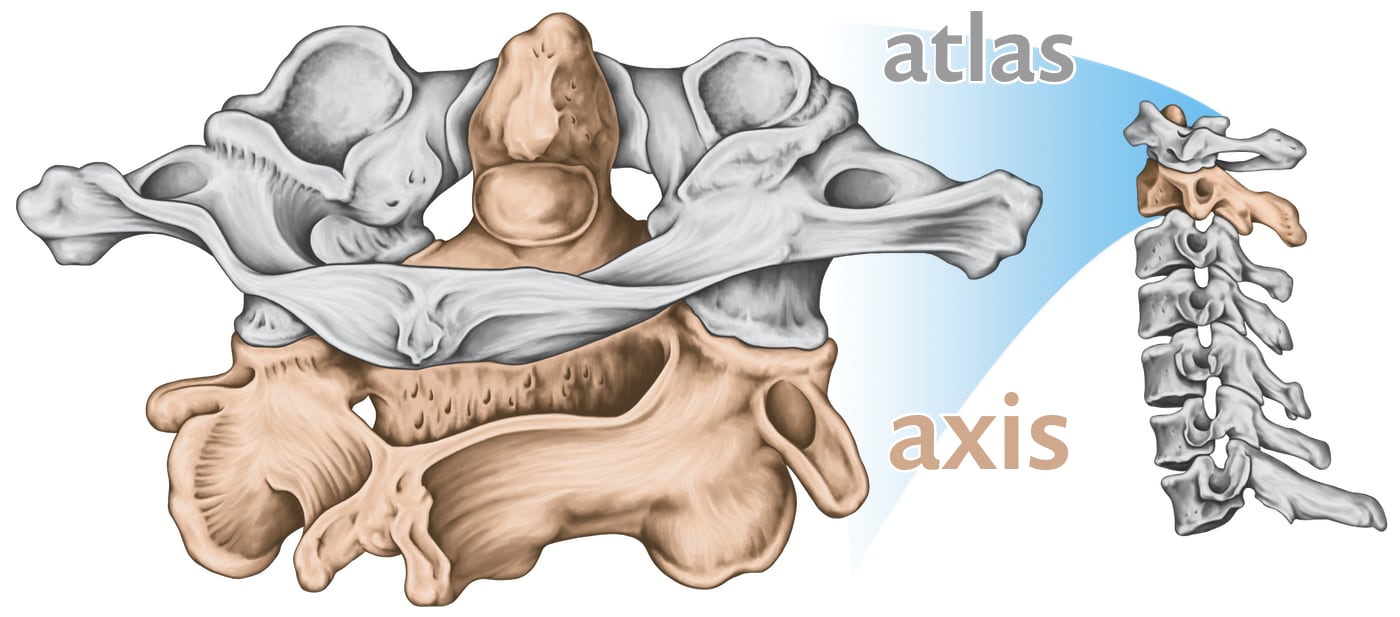
These are the first and second cervical vertebrae — the “atlas” and “axis” — with the peculiar finger-like projection of the axis (the “dens”). It sticks upwards into the ring of the atlas above it … and it shares that small space with the brain stem. It is normally strapped to the side of the ring by a tough ligament. But if that ligament loosens or breaks … 😬
This rogue piece of bone, called the dens, is normally held down by a strap of ligament, which is sometimes broken in accidents, or eroded and loosened by some kinds of arthritis, or by cancer. His severe chronic neck pain and headaches — the reason he went for a massage in the first place — could be the result of his neck muscles working tirelessly to keep everything stable. His body knows — even if he doesn’t — that this is a life-threatening situation!
AAI is a complex condition, with many possible causes. It does not necessarily cause any distress. Even patients with severe instability may have no symptoms at all, while others with relatively minor instability experience significant problems.3 Nor is it actually possible to reliably diagnose AAI by feel,4 as I was trained to do.
So it may well be possible for patients with AAI to lead normal lives, and if they suffer from chronic neck pain or headaches they can probably be treated cautiously with massage therapy — but it is crucial that they understand the nature of their problem. They are clearly vulnerable, regardless of whether they have obvious symptoms, and careless massage therapy and spinal manipulation are obviously dangerous. Athletic activities like skiing need to be reconsidered when a mild fall could end your fun forever!
Could it have been a case of artery damage?
In addition to the large carotid artery, small arteries in the side of the neck supply the brain with blood. These arteries are somewhat vulnerable to being pinched off or even torn. If the flow of blood is impaired, it’s called vertebrobasilar insufficiency, or VBI. If the artery actually tears, which can cause brain damage due to the loss of blood supply to the brain, it’s called vertebral artery “dissection,” or VAD.

VBI/VAD can also cause the kinds of symptoms my barber had, and worse — even death. Also, alarmingly, sometimes it only causes pain, which is disturbingly little indication of a very serious problem. This isn’t common, but it’s not rare either.5
It’s somewhat unlikely in my opinion that this was the cause of my barber’s terrible experience: dizziness and vomiting are more typical of brain stem lesions. His history of severe neck tension and headaches tends to point towards atlantoaxial instability. And the lack of other typical VBI/VAD symptoms is also an indicator. VBI is more likely to cause persistent symptoms in a variety of circumstances. VAD is often even more serious than what he experienced, although there is such a thing as a “small” stroke (even asymptomatic ones).
There’s no way to know for sure, of course.
But whatever happened, it was for damn sure not “toxins” being “released” by massage!
Can chiropractic adjustment do this also?
Evidence suggests that cervical spinal manipulative therapy — neck cracking — might be dangerous, with minimal benefits to justify the risk. Not only can chiropractic adjustments of the neck be dangerous for people with atlantoaxial instability for obvious mechanical reasons, neck adjustments are also “associated with” VBI/VAD,6 as well as a fairly high rate of less dangerous but still rather unpleasant side effects.7
Pain may be the only symptom these vulnerable patients have — and yet, ironically, they seek the kind of treatment most likely to cause much greater harm. Both patient or chiropractor may not realize the nature of the pain until it’s too late.8
Experts actually mostly agree on this topic. Even chiropractic authorities acknowledge that “there are considerable case studies describing the onset of vertebral artery injury following a manipulation.”9 The infamous Cassidy paper says otherwise, but doesn’t make its case nearly as strongly as chiropractors would like to believe.10 There is more legitimate controversy about whether neck adjustment actually causes neck disasters.
Athough the risk of such serious complications probably is low, it must be considered, because the benefits of joint cracking in the neck are not clear — not for neck pain,1112 not for headache13 — either and chiropractors often perform neck adjustments for reasons criticized by most doctors and even many chiropractors.14 “If the risk is death and the benefit is zero, then it is unacceptable to proceed.” Or, as a group of Canadian neurologists put it, “Is a headache worth dying for?”15
Massage therapy for the neck, at least, is less dangerous and probably more beneficial — at the very least, it can be pleasant and relaxing. As long as a loose vertebrae is not disturbed!
Just as with my barber’s massage therapist, the dismissive attitude that chiropractors sometimes have about these hazards can be quite disturbing. Consider this story that I came across not long after hearing my barber’s story. Please note that this anecdote was originally published by a chiropractor:
Following manipulation the patient said, “Oh, that was awful, something terrible has happened to me. That’s awful. Let me up. I don’t want anymore; I can’t stand anymore.” The chiropractor then said “you will be all right. Let me get this other one.” The patient then said “I have had enough, don’t, stop.” The chiropractor continued to manipulate the patient. Immediately following the adjustment she was unable to walk, her vision was impaired, she vomited, and she had a partial paralysis of the throat and vocal cords.
Vertebrobasilar stroke following manipulation, by A Terrett
Why did my barber’s therapist fail?
My barber’s therapist probably failed because he was, like most massage therapists, simply not well-trained enough to know any better, despite the unusually high certification standards for massage therapist in this part of the world.16
The state of the art is a moving target, and I was taught obsolete information. I learned the basic manual tests for AAI in school in 1998 or so, a couple years after Swinkels et al. had already published a review showing that the tests were unreliable.
The idea of such testing is to basically just to cautiously feel for the looseness of the joint, and to watch for the signs of brain stem impingement. In theory, we were taught the tests so that we could identify patients that might be accidentally injured or killed by careless manipulation of the neck — an extremely important safety issue!
And yet I don’t remember any particular emphasis being placed on the testing, and I do clearly remember being alarmed that I graduated with several students who didn’t really seem to “get it.” What a thing not to “get”! This ignorance was particularly surprising given that we’d had some dramatic personal exposure to the issue: one of our own classmates actually had symptomatic post-traumatic AAI and was actually injured by another classmate in our student clinic, someone who didn’t even have to do the testing, because the patient walked in the door and said, “I have AAI. If you’re not careful with my neck, I’ll throw up for a day, and you could kill me.”
And it still happened. She was still carelessly treated, threw up, and was a wreck for a day or two.
I became the only student in the class that student would accept treatments from, I am proud to say. She recognized that I was aware and cautious enough to trust.
Today, one of my own clients has the same condition, and he also receives safe and effective treatment from me in spite of this extraordinary risk. So I have some first hand experience with this condition. The tests may be unreliable — especially because of therapist incompetence — but the warning signs are fairly clear.
When starting to treat someone with AAI, an alert therapist should sense that something is not right: they will notice an ominous combination of case history clues, perhaps combined with unusually guarded movement of the neck and high tone in the neck muscles. Once that concern is triggered, a therapist must switch into better-safe-than-sorry mode. And why not? No harm is ever done by slowing down and easing up! All therapists should do so whenever they encounter certain signs.
It is still possible to miss the problem, though. Not every case is severe or symptomatic, and the work is complex — what if the patient doesn’t even have a history of odd AAI-ish problems? Or what if the patient doesn’t take his or her symptoms seriously and doesn’t report them? Patients will often minimize or even conceal important clues, for all kinds of reasons.
The unforgiveable failure in my barber’s case was what he was told by his therapist after reporting a nasty negative reaction. Why would a Registered Massage Therapist brush off such severe consequences of a treatment? I leave it to your imagination, with the reminder that not everyone can graduate at the top of the class, and someone has to graduate at the bottom.
Even a barber knows that a neck massage shouldn’t make you throw up. He never went back. Thank goodness.
Licensing is not enough
This is depressing to contemplate, but it contains an important lesson for health care consumers: not only is it important to seek health care services only from licensed professionals, you must do your best to discriminate between the good ones and the not-so-good ones. Licensing alone does not guarantee skilful and responsible health care!
It’s a frustrating reality of our system that marginalized alternative health care professionals must compete in the marketplace in order to make a living, which undoubtedly skews our judgement from time to time. I know from personal experience that it can be difficult to be objective when I am trying to pay the rent. However, good therapists quickly build up a large enough clientele that this ceases to be a problem, and even in my first year I was never so desperate that I compromised the safety of my clients by ignoring ominous symptoms.
So what’s a customer to do?
Here’s a quick checklist of things to watch for, and things to avoid. It applies specifically to massage therapists, but many of them also apply to any health care professional, especially physiotherapists and chiropractors.
| 👍🏻 | 👎🏻 |
|---|---|
| Case history form | No case history form (very bad sign) |
| Detailed interview | No interview or minimal interview (another very bad sign) |
| Relaxed and comfortable asking you questions | No physical assessment (not necessarily a big deal, but still questionable) |
| Some kind of physical assessment, even if the issue seems simple | Treatment is immediately intense |
| Treatment is cautious and conservative initially, and never causes wincing or gasping or gritting of teeth | Treatment intensity is hard to cope with |
| Therapist focus is initially broad, checking in with the whole body | Therapist doesn’t ask how you’re doing, or ask for information about your experience of the treatment |
| Therapist communicates with you and asks for feedback about sensations, especially in the first appointment | Therapist ignores basic comforts such as temperature, volume of the music, positioning on the table, etc. |
| Therapist shows obvious concern for your comfort with the experience in general | Narrow treatment focus (zooms in immediately on the problem area and pays no attention to anything else) |
| Therapist explains things to you clearly | pseudoscientific buzzwords and excessively flaky explanations |
| Explanations sound sensible to you | Or, even worse, no explanations at all |
| No pressure to rebook, just a prognosis and a range of options to choose from | Pressure to rebook |
An activator incident: can a light tap injure the neck?
Chiropractic “activators” are tiny spring-loaded “hammers” that “tap” the spine to “adjust” it. They can definitely waste your time and money, but … can they hurt you? Just a little tap? A reader asked:
A chiropractor hit my C2 vertebra with an activator, and I’ve been dizzy/nauseated for 3 months since then. Could a gentle tap on the cervical spine cause this?
Maybe. It would be a bit of a freak accident, but freak accidents happen. I think it’s possible — and worth thinking about how it might work.

Not actually a chiropractic “activator” … but a bizarre AI-generated depiction of one. The real thing is much tamer, with a rubber business end. This image is typical AI slop, obviously a “creative” mashup of several small tools. I have tried using AI for a lot of simple images, and it just sucks at realistic depictions of specific objects. This is the best I could get after extensive experimental prompting to make the image more accurate. 🙄 The result is abstractly amusing and fascinating — I love how tool-esque it is, without actually resembling any specific tool — but it’s completely useless. If you want to know what a real chiropractic activator looks like, search for it! I used this image “because copyright,”17 and just for fun.
We know from all of the above that spinal movement can go badly, we can extrapolate from those examples, and it is plausible in principle that even minor passive manipulation of the upper cervical spine could cause some trouble. The difference between passive neck manipulation and active neck movement is the key here:
Passive cervical manipulation is anything that is done to your neck — movement of tissues that you didn’t initiate.
Active movements, of course, are the movements you control — with all the details unconsciously micromanaged by your brain on your behalf, in service of your high-level commands. “Look over there” involves an army of details. You don’t have to think about what to do with your rectus capitis posterior minor muscle, thankfully.
When your neck movements are up to you, your body makes accurate, rapid, and even aggressive compensatory adjustments to protect you from a vulnerability, such as instability or a position that irritates nerve tissue. Some people probably go their whole lives “working around” such vulnerabilities, never even knowing they exist.
Such stealthy vulnerabilities could still cause symptoms occasionally, because perfect protection always possible for this system. Accidents happen! But mostly … it just works.™
But deliberate and novel passive manipulation might surprise the brain, imposing movement on a vulnerable spine that it never would have permitted in active movement.
A chiropractic “activator” could conceivably be an example of this in principle, but it would be surprising if it could do much damage in practice — it’s probably too gentle. Skeptics and critics justifiably make fun of how clinically trivial they seem, because they do so little physically that it’s highly implausible that they can be therapeutic. But that means it is equally implausible that they can do harm.
And yet not impossible. If you’re close to the edge of a cliff, it doesn’t take a big push to slip over it. It would take a perfect storm, but that active/passive distinction is important, and I can imagine it combining poorly with a particularly delicate vulnerability, and more aggressive use of the activator.
•
Or it was all an illusion! Maybe the activator wasn’t the active ingredient in my reader’s misfortune. The true culprit could be passive neck movement before and after the activator usage! 🤷🏻♂️ That’s probably more likely. But I do think activators have at least a little bit of potential to do harm — beyond wasting your time and money, that is.
See also: Chiropractic with a hammer. Not all spinal tapping is gentle!
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Related Reading
- Does Massage Therapy Work? — A review of the science of massage therapy … such as it is
- How Do Your Find Good Quality Massage Therapy? — Tips for finding good quality medical massage, and avoiding nonsense and quackery
- The Chiropractic Controversies — An introduction to chiropractic controversies like aggressive billing, treating kids, and neck manipulation risks
- Does Spinal Manipulation Work? — Spinal manipulation, adjustment, and popping of the spinal joints and the subluxation theory of disease, back pain and neck pain
What’s new in this article?
Jan 7, 2025 — New section, “An activator incident: can a light tap injure the neck?”
2024 — Added a good quality diagram of artery dissection.
2020 — Minor addition of a definition of beauty parlour syndrome.
2017 — Added information about artery tears with pain as the only symptom.
2016 — Minor update to references related to SMT for headache.
2005 — Publication.
Notes
- Mild toxemia following massage therapy is possible, but also pretty trivial: the body might do some “metabolic housecleaning” when stimulated by manual therapies. However, the symptoms are generally limited to headaches, fatigue, loginess and (in the worst cases) allergy-like symptoms. In short, nothing even remotely approaching the severity of the side-effects my barber experienced!
- It’s a poor quality name, because it doesn’t fit the definition of a “syndrome” well at all. A syndrome is an unexplained pattern of signs and symptoms that is distinctive and common enough to deserve a descriptive name before we can technically diagnose it. But beauty parlour syndrome isn’t unexplained! It’s a stroke, and we know how it’s happening.
- In 1996, Swinkels reported that “There is no correlation between the measure of hypermobility and the presence of clinical symptoms.”
- Swinkels also report that “the validity of the upper-cervical stability tests is questionable” and in 2008 this was reiterated by Mintken: “ … there are very few data to inform and guide practitioners on the use of ligamentous stability tests when assessing the upper cervical spine.”
- Pain may be the only symptom in 10-60% of cases. Lower numbers are given by Arnold 2006, Kerry 2009, Maruyama 2012. Bogduk goes to 60%, which seems like a crazy outlier, but it may be fair and the exact number probably depends on how long it has been since the VAD. Fresher cases are much more likely to seem like a normal headache; the symptoms evolve over time.
- Smith WS, Johnston SC, Skalabrin EJ, et al. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology. 2003 May 13;60(9):1424–1428. PubMed 12743225 ❐
From the abstract: “This case-controlled study of the influence of spinal manipulative therapy and cervical arterial dissection shows that spinal manipulative therapy is independently associated with vertebral arterial dissection, even after controlling for neck pain.” Cervical arterial dissection is when one of the two arteries that wind through the back of the neck to the brain start to tear. The lining of the artery bleeds and forms a blood clot. This clot can easily enter the brain and cause a fatal stroke.
- Carlesso LC, Gross AR, Santaguida PL, et al. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: A systematic review. Man Ther. 2010 Oct;15(5):434–444. PubMed 20227325 ❐ Increased neck pain might be 25% more likely with SMT than if you did nothing or stuck to safe and neutral treatments (but that chance of risk was also statistically insignificant, and the authors actually took it to mean that there probably are no negative reactions — a fair point, but also a debatable one). Much more definitely, patients are 100% more likely to have “transient neurological symptoms,” which can range from dizziness all the way up to serious unpleasantness, such as severe dizziness, nausea and vomiting. (These are relative risk measurements: the risk compared to not getting treated — not the overall likelihood, which cannot be measured from this kind of data.)
- Maruyama et al.: cervical dissection pain is “often interpreted initially as migraine or musculoskeletal in nature by the patient or the treating doctor.”
- National Chiropractic Mutual Insurance Company [Internet]. Triano JJ, Kawchuk G, Gudavalli MR, et al. Current Concepts: Spinal Manipulation and Cervical Arterial Incidents 2005; 2005 [cited 23 May 15]. PainSci Bibliography 56048 ❐
- Cassidy JD, Boyle E, Côté P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008 Feb;33(4 Suppl):S176–83. PubMed 18204390 ❐
Since its publication, “the Cassidy paper” has been the defensive citation used by chiropractors to respond to accusations that neck adjustments involve a risk of stroke, and therefore should not be conducted without proven benefit and informed consent. The abstract seems to strongly exonerate chiropractors: “We found no evidence of excess risk of VBA stroke associated with chiropractic care compared to primary care.”
“But abstracts are like movie trailers,” as Dr. Mark Crislip wrote. “They give a flavor of the movie, but often leave out many important plot devices and characters. … If you were to read this article in its entirety, you would not be so sanguine about the safety of chiropractic.” He goes on to explain exactly why in one of the earliest popular posts on ScienceBasedMedicine.org, Chiropractic and Stroke: Evaluation of One Paper.
What chiropractors take from the paper is that the strokes that follow cervical spinal manipulation were already in progress, causing the symptoms that inspired the appointment. That is possible, but it is only one possibility, and the paper’s abstract emphasizes this hypothesis like it’s a conclusion (and most people stop reading when they are told what they want to hear). That hypothesis is not supported by the data Cassidy et al. pulled together (which has some key flaws). And there are other ways to explain the data. Dr. Crislip’s conclusion “from reading the paper in its entirety, rather than the abstract”:
A population that should not have a stroke, the young, has a marked increase association with stroke 24 hours after visiting a chiropractor and that given the rarity of a vertebral artery dissection as a cause of stroke in the elderly, the elderly is not a group that one could easily find an increase in stroke after chiropractor visit.
- Back in 1996, Hurwitz wrote that “cervical spine manipulation and mobilization probably provide at least short-term benefits for some patients with neck pain and headaches.” Not exactly a glowing endorsement. But more recent and thorough reviews of the literature have been even less enthusiastic. In 2004, Bronfort wrote in Spine that, “There are few studies, and the evidence is currently inconclusive,” and that for chronic neck pain mobilization/manipulation “offers at most similar pain relief to … rehabilitative exercise in the short and long term.” Going from bad to worse, in 2006 Spine published an even more authoritative review of the scientific literature from The Cochrane Collaboration, concluding that neck adjustments are “not beneficial” when used alone (it did qualify that there was evidence that neck adjustments could work when combined with exercises, which doesn’t exactly make it sound like a miracle cure).
- Dr. Nikolai Bogduk weighs in with a paper with his conclusion right in the title: “Spinal manipulation for neck pain does not work” I take Bogduk’s opinion very seriously, as he is one of a small group of elite pain scientists in the world today, whose opinions are relentlessly well-informed and sensible. This guy is smart, and if he says neck adjustment doesn’t work, he’s got a good reason for it.
- Unfortunately, the evidence with regards to headaches is even scantier. There were inconclusive scientific reviews of almost no good evidence in 2004 and 2007, and no improvement in 2011 in the most recent credible review (Posadzki): “There are few rigorous RCTs testing the effectiveness of spinal manipulations for treating cervicogenic headaches. The results are mixed and the only trial accounting for placebo effects fails to be positive. Therefore, the therapeutic value of this approach remains uncertain.” One more recent trial had positive results (Espí-López) but I don’t trust them. For a more detailed analysis, see The Complete Guide to Chronic Tension Headaches.
- Many “straight” (old school) chiropractors continue to treat the spinal joints because they believe that spinal adjustment can cure all kinds of health problems. This is inconsistent with everything known about anatomy and physiology, and has been debunked by countless experts. See my article The Chiropractic Controversies for a summary of the issues and evidence, or read Inside Chiropractic for an excellent critique of the chiropractic profession written by a chiropractor.
- Neck911.com [Internet]. Statement of Concern to the Canadian Public from Canadian Neurologists Regarding the Debilitating and Fatal Damage Manipulation of the Neck May Cause to the Nervous System; 2009 [cited 09 Jul 19]. PainSci Bibliography 55499 ❐
- BC is the only place in the world where you can get 3000 hours (3 years) of training to be a massage therapists — roughly three times more than most places, and even 6 or 8 times more than many places. Until a recent change in legislation, 3 years was the requirement for certification.
So why didn’t I use a real activator picture? I could have! I have used product images in my posts from time to time because — although technically violating someone’s copyright — the copyright owner is rather unlikely to be unhappy about it. Indeed, if you link to the product, they may even see it as a favour.
But it’s a grey area, and certain kinds of products and copyright holders are best avoided … and/or I don’t want to “endorse” them. Chiropractors are notoriously thin-skinned and litigious as a group — which I have learned the hard way — and so I chose not to risk even a tiny provocation over an image that isn’t terribly important to the post. But I still wanted some kind of image!
