IT Band Pain is Knee Pain, Not Hip Pain
Pain in the hip and thigh is something else, I promise
Can hip pain be “IT band syndrome”? Does IT band pain ever affect the hip? This a chronic point of confusion about iliotibial band syndrome (ITBS) — where exactly does it actually hurt? Many professionals incorrectly diagnose hip and thigh pain as ITBS. There is no such thing as non-knee ITBS. By definition,1 ITBS occurs only on the side of the knee. More specifically:
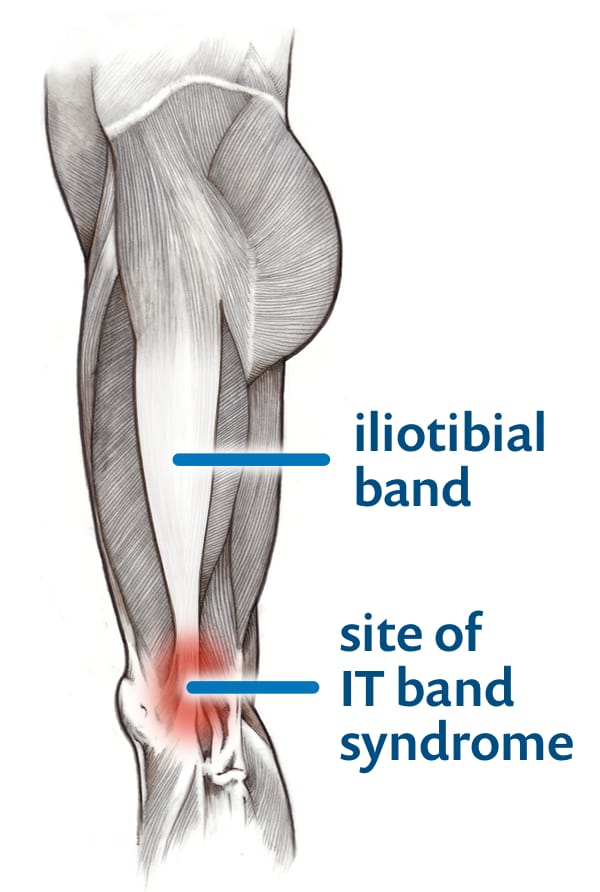
- the outward-facing side of the knee
- at or just above the prominent bump of bone (lateral epicondyle)
- well-defined pain location, an epicentre you can point to with precision
- fairly superficial — on the side of the knee joint, not in it
The condition is caused by the irritation of tissues around that anatomy. Pain anywhere else — like the thigh and hip — is something else. I promise. I’m not making this up. I’ll have more to say about diagnosing IT band pain below, but first…
So what does cause hip pain?
Nothing is mistakenly called ITBS more often than hip and thigh pain, which can be just as stubborn and baffling as ITBS. Calling it ITBS implies that it has something to do with the IT band, when in fact this kind of pain has many and likely overlapping causes.2
IT band syndrome is a “syndrome” because the pain is unexplained. We don’t know the specific mechanism, so we don’t give it a name that implies a specific cause (like “tendinitis,” for instance). All syndromes are simply descriptions of an unexplained but distinctive pattern of symptoms. Most syndromes involve patterns of symptoms with a lot of variation, but the pattern of ITBS is more simple and specific: pain on the side of the knee, related to overuse, notably aggravated by descending stairs and slopes. It’s only unexplained insofar as no one has quite figured out exactly what tissue gets into trouble.8
But ITBS is not unexplained hip pain. It’s unexplained knee pain.
There are many known causes of hip pain, of course. But for puzzling lateral hip pain with no other obvious explanation — which is quite common! — you need another syndrome …
Greater trochanteric pain syndrome (GTPS)
The standard label for undiagnosed, generally lateral hip pain is “greater trochanteric pain syndrome” (GTPS), and the pattern is: aching with an epicentre around the large bump of bone on the side of the hip, the greater trochanter of the femur. While this is usually experienced as “mainly” hip pain, it also often involves widespread, diffuse pain throughout the entire region and into the thigh.
GTPS is often mistaken for IT band syndrome, probably mainly because the pain spreads down into the thigh just where the big IT band tendon happens to be.
While GTPS is usually mostly about the hip, it also often involves widespread pain in the low back, throughout the glutes, and down the side and back of the leg as well. It is a distinct condition in its own right, and yet it probably often has overlapping causes, for instance both referred pain from lumbar spinal problems and some cluneal nerve entrapment.
Now let’s look at some of the more specific causes mechanisms of hip pain …
Arthritis as a cause of hip pain
One of the most common assumptions about hip pain is that it must be arthritis. But concern about arthritis is rarely justified: most people with signs of arthritis (on X-ray) do not have any pain, and most people who have hip pain do not have arthritis.3 Obviously hip arthritis is a thing, but rarely under the age of 50, and rarely in the very active runners who most often get ITBS.
And yet! When hip pain does happen in someone who might also get ITBS, confusion is possible. Deep hip joint pain is routinely felt all over the hip and buttocks, and can easily be confused with the shallower pain of GTPS. A hollering hip joint can send pain deep into the thigh as well, especially the lateral thigh all the way down to the knee (and even lower), which also makes it surprisingly likely to be mistaken for IT band syndrome.4 Referred pain is always good for some diagnostic hijinks.
Muscle as a cause of hip pain (and there’s probably a lot of that)
The most common cause of hip pain, especially in younger patients, is probably just the aching and stiffness associated with “muscle knots,” sore spots known as trigger points (TrPs).5 The TrPs themselves are usually in the hips, but the pain often spreads (“refers”) downwards into the thigh.6 A common and easy example of this phenomenon is Perfect Spot #6: the TrP is in the upper hip, but the pain spreads into the back, buttocks, and thigh. Another important example is the common trigger point in the tensor fasciae latae muscle.7
Hip muscle pain is not only a common problem in general — with or without ITBS — but also potentially implicated in ITBS. For instance, grouchy hip muscles that control the tension on the IT band might be a minor factor causing ITBS. Many ITBS patients seem to experience significant hip discomfort in addition to their strong lateral knee pain. Treating the hip pain may or may not have any effect on ITBS, but is probably worthwhile in itself.
If you think that you might have hip muscle pain, my muscle pain tutorial should be your next stop.
Of pain sources in the leg itself, the big quadriceps trigger point in the vastus lateralis — right under the IT band — is a common doozy, Perfect Spot #8. That pain tends to dominate the lower end of the thigh.
Other pain locations and types that are not IT band syndrome
We’ve talked about other major causes of hip pain. Let’s move on to other not-ITBS pain types in the thigh, knee, and lower leg, some of which might involve the iliotibial band, but still are not “IT band syndrome” per se.
Many of these conditions cause diffuse or complex knee pain that sometimes includes the side of the knee, but in most cases what distinguishes it from ITBS is that you can't point to the side of the knee and say, "This is where it always hurts the most." If the pain is hard to precisely locate, or it moves around, or it's definitely something else. ITBS is not hard to locate!
Once more with feeling: no prominent hot-spot on the lateral knee, no ITBS diagnosis!
But here are some of the other conditions that can mimic ITBS to some degree, or just co-exist with it, because of course there's nothing about ITBS that eliminates the possibility of other painful conditions in the knee and nearby.
Patellofemoral pain syndrome and ITBS vs PFPS
This is the big one, the other very common cause of load-related knee pain in younger people, and the pain is right next door. It’s also often known as AKA patellofemoral pain syndrome (PFPS) because it's often unclear if it’s related to the patellofemoral joint itself, or underlying deeper structures — and so it gets "syndrome" stuck on it.
Which condition is “runner’s knee” — ITBS or PFPS? Trick question: they both are. They are constantly confused because they are both common repetitive strain injuries of the knee, causing pain in locations that are anatomical neighbours.
But they are simple to distinguish in principle: ITBS causes focal pain on the side of the knee, and PFP is all about more diffuse pain on the front of the knee, and
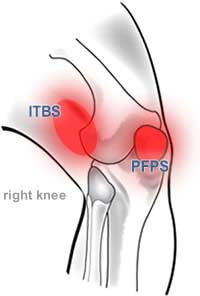
Where’s the pain?
IT band syndrome dominates the side of the knee. Patellofemoral pain is more variable, but usually more in front.
I have a an entire article about how to tell these two apart: Diagnosing Runner’s Knee: It usually starts with lateral knee pain during and after runs, but there are two major types.
Stress fractures of the lateral epicondyle
These fractures can be quite sneaky and hard to diagnose, and might cause some lateral knee pain in addition to plenty of diffuse, deep pain. However, the lateral pain component wouldn’t be vivid, specific, superficial, and independent enough for an ITBS diagnosis to make much sense.
Knee arthritis
Knee arthritis is rarely hot on the side of the knee specifically, it generally doesn't behave like an overuse injury, doesn't typically have the same "hot side of the knee" signature, and mostly isn't likely in the relatively young, active people that get IT band syndrome.
But cases of ITBS do crop up in older people, especially after knee surgeries or other injuries, and may be much harder to tell apart from arthritis.
Lateral meniscal tears
Another source of pain on the outside of the knee, but it’s usually caused by an obvious injury, with pain a little too low and too deep for ITBS, and usually accompanied by other signs and symptoms like swelling, locking, clicking, and clunking.
Posterior knee pain
Posterior knee pain has several possible specific causes, like popliteal artery entrapment syndrome (PAES), popliteal or biceps femoris tendinopathy — but it’s clearly or mainly posterior pain, it’s definitely not IT band syndrome. Nevertheless, I have seen all of these conditions get carelessly misdiagnosed as ITBSProximal tibiofibular joint pain: a little lower
When injured, this obscure joint — not quite part of the knee — does cause “lateral knee pain” and is often misdiagnosed as the far more notorious ITBS. However, the pain location is distinctly below the knee joint, and usually begins with an obvious trauma (dislocation and sprain). For more information, see The Tibiofibular Joint and Knee Pain.

Lots more reading about IT band syndrome
These are all of the free excepts from my book about IT band syndrome available on PainScience.com. It’s a lot, but it’s only about 20% of the entire book.
- EXCERPT IT Band Stretching Does Not Work
- EXCERPT Does the IT Band Move After All?
- EXCERPT The Causes of Runner's Knee Are Rarely Obvious
- EXCERPT Do IT Band Straps Work for Runner’s Knee?
- EXCERPT How I Recovered from IT Band Pain, Eventually
- EXCERPT Is IT Band Tendinitis Really a Tendinitis?
Or just start reading the free introduction to the IT band syndrome book. If you find the free content useful, consider buying the book, or a donation to support user-friendly evidence-based publishing.
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the Internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
What’s new in this article?
2023 — Added information about hip joint pain mimicking other kinds of hip and thigh pain.
2019 — Heavily revised with a much stronger focus on differential diagnosis. I think the perspective makes the article much more useful.
2017 — Science update — Cited evidence of poor correlation between hip pain and radiographic signs of arthritis (Kim et al.).
2017 — Miscellaneous minor improvements. Very careful clarification of the symptom location. Migrated some details to footnotes, and added some details specifically for footnotes.
2010 — Publication.
Notes
- There’s nothing formal or authoritative I can cite to support this position; there is no international standards organization defining minor musculoskeletal injuries; IT band syndrome isn’t even in the Merck Manual (a famous medical dictionary) or the Medline/Merrian Webster medical dictionary. All obscure definitions are somewhat arbitrary and a product of social concensus, and so my position is based on the definition used in most academic writing and research on the topic. My strong impression after many years of writing about ITBS is that discussions and articles that conflate hip and proximal thigh pain with knee pain are mostly amateurish, with ignorance of the condition prominently on display.
Why would anyone call hip pain ITBS? Two reasons:
- the IT band is long and it is part of the hip as well as the knee
- hip pain can spread well down the thigh, as far as the knee, sometimes even beyond
- Kim C, Nevitt MC, Niu J, et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ. 2015;351:h5983. PubMed 26631296 ❐ PainSci Bibliography 53332 ❐
This analysis of thousands of patients confirmed a jarring disconnect between signs of arthritis on hip x-rays and hip pain: “Hip pain was not present in many hips with radiographic osteoarthritis, and many hips with pain did not show radiographic hip osteoarthritis.” What they mean by “many” is “practically all”: roughly 80% of patients with signs of arthritis had no pain, and at least 85% of patients with hip pain had no sign of arthritis! These numbers held up even at the extremes — most older patients with a high suspicion of hip arthritis did not in fact have arthritis that could be diagnosed with an x-ray.
- Lesher JM, Dreyfuss P, Hager N, Kaplan M, Furman M. Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9(1):22–5. PubMed 18254763 ❐
Conventional wisdom says hip joint pain usually refers to the groin and thigh, and both of these are common (each seen in about half of patients)… but investigating this phenomenon Lesher et al. found that buttock pain is even more common at 70%, and even lower leg pain is also surprisingly common at 20%.
Foot? 6%! Imagine that one. “Doctor, my foot hurts.” “Hmm, could be hip trouble…”
Knee? 2%?
So there is real potential to mistake hip arthritis for other issues, especially sciatica and greater trochanteric pain syndrome.
Location Percentage of Patients Buttock 71 Thigh: 57 Anterior 27 Lateral 27 Posterior 24 Medial 16 Groin 55 Leg 16 Lateral 8 Posterior 8 Anterior 4 Medial 2 Foot 6 Knee 2 - This assertion is based primarily on my decade of clinical experience as a massage therapist, seeing many cases of hip pain attributed to things like bursitis or arthritis that were readily resolved with a little massage. It’s also just all that’s left after a relatively simple process of elimination: many of the “usual suspects” in the hip have distinctive clinical characteristics that simply aren’t present in most cases. And finally it’s based on my confidence that trigger points are a genuine ubiquitous clinical phenomenon, which no one disputes, even if their nature is controversial: see The Trigger Point Identity Crisis.
The brain is somewhat inept at precisely locating internal pain and so sometimes we experience pain in a broad area around or near the cause, or even further afield. This is the same phenomenon as heart attack pain felt mainly in the arm: the brain just can’t figure out where the pain is coming from, and the arm pain is a bad “guess.” Patterns of referral from the musculoskeletal system are somewhat predictable, and most referred pain spreads away from the centre and the head (laterally, distally). By contrast, visceral referral is much more erratic.
This phenomenon is probably one reason the IT band gets blamed for hip pain. The referred pain from the hip simply spread down the side of the thigh, where the IT band happens to be.
- Which is harder to describe and self-treat. It is about the size of a large pickle and “hangs” straight down from the side of the prominent bump of bone on the front of the hip, the anterior superior iliac spine.
- For instance, it’s probably not “friction” of the IT band, a kind of tendinitis, as implied by the common term “IT band friction syndrome.” See Is IT Band Tendinitis Really a Tendinitis?
