Magnesium supplementation as a pain killer
The things that normal people use to self-treat their pain are rarely tested in good clinical trials. Today’s example: magnesium supplementation for chronic pain. Can it actually help patients? Is it basically a pain-killer? And shouldn’t we know that for sure by now?!
Of course we should! But of course we don’t. In this post, I’ll look at some of the scraps of science we do have, and the salamander will make some recommendations.

Magnesium crystal. Some processing required before ingestion.
But why? The rationale for magnesium supplementation
It’s a popular idea that magnesium deficiency is a significant factor in many cases of chronic pain. This is one of the main reasons people literally bathe in the stuff (Epsom salts are magnesium sulfate). The magnesium-pain hypothesis has some seeds of truth. For instance, deficiency is somewhat common (even though it’s easy to eat). And it’s clearly a staple molecule in neurology. I discuss this in more detail in my supplements review, and the Epsom salts article digs it with a focus on absorption.
Pain relief via cramp relief is another possibility: a little more on this below, and bunch more in my big cramps and spasms review.
Testing magnesium with a keyboard and mouse
A 2020 study seemed to go out of its way to try to answer this question without actually talking to a patient with pain — pure data analysis. Tarleton et al mined some old survey data on the health of more than 13,000 American adults (high-volume data, but also poor quality for this purpose, “low resolution”). They reported a “protective effect” of “increased magnesium intake,” concluding that this “warrants further study.”
Which everyone more or less already agreed on, but more data is good… right? Hm, not if it just muddies the waters. Data like this is can be like yelling in a crowded theatre, “There might be a fire! I think I saw some smoke!”
But this is a far cry from conclusive evidence that taking magnesium treats any kind of chronic pain. This alleged protective effect of “increased magnesium intake” is inferred from notoriously unreliable self-reporting of diet. The possibilities for confounding factors are endless.
Not a great paper.
Bonus eye roll: Amusingly, when Tarleton et al explained why they did this research — that “there is some evidence that magnesium supplementation results in improved pain management” — they cite only a single supporting paper. And what is that single paper? A twenty-year-old study showing an inflammatory response to severe deficiency… in rats. 🙄

It’s easy to eat magnesium. You just have to be willing to eat salad. Or potatoes!
A Canadian review of not much magnesium science
Banerjee et al concluded in 2017 that “magnesium appears to have an analgesic effect.” Hooray? But don’t read the fine print if you want to hang on to that good feeling.
Their own summary of findings doesn’t seem to back up the optimism. They state that conclusions were “not possible” for migraine … that the evidence is conflicting for a rather exotic kind of chronic pain (complex regional pain syndrome) … and they mention only a single trial showing a benefit for back pain (coming up below). If there is enough evidence to justify “magnesium appears to have an analgesic effect,” it is not reported here.
Also not a great paper.
One of the few good trials of magnesium for pain
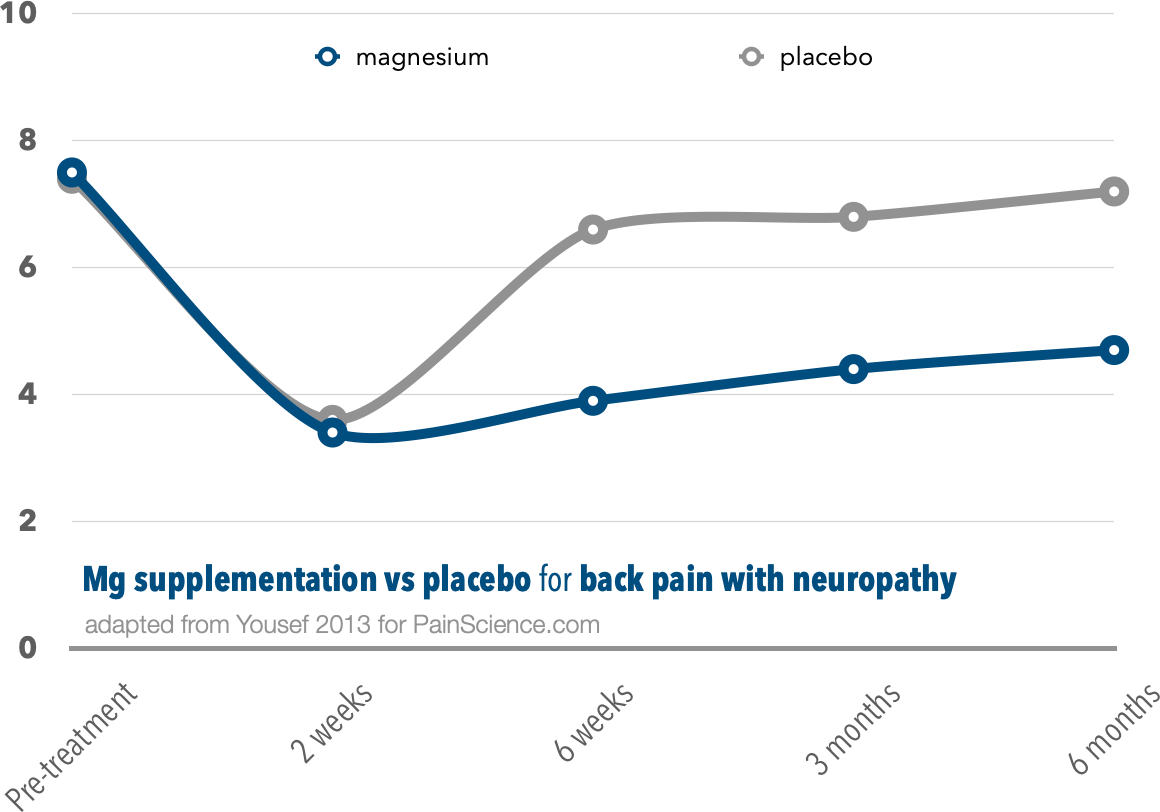
Yousef et al did a true trial of magnesium supplementation for back pain — but, crucially, only back pain with a neuropathic component. 40 patients got intravenous magnesium for two weeks, then oral for another month, and their progress was compared to 40 patients who got a placebo in the same ways.
The patients who got magnesium clearly did better in the long run.
Both groups did great at first, more than halving their pain. If stopped there, the study would have shown that magnesium was no better than a placebo. But then the placebo group’s numbers rebounded, while the magnesium folks stayed low… for six months. The improvement wasn’t huge, but it wasn’t small either. I wouldn’t turn it down.
It’s “just one study,” with unknown flaws, and still unreplicated as of 2024. Most important, this experiment just cannot tell us anything about the effect of magnesium on the most common kinds of pain, which are mostly not neuropathic. But it’s still a noteworthy positive result.
What about painful cramps?
You will get told to take some magnesium for your cramps … even though many kinds of cramps aren’t caused by magnesium deficiency, and magnesium deficiency doesn’t clearly cause cramps! A 2020 review was all thumbs down for treating cramps with magnesium, except for a ray of hope about pregnancy cramps (Garrison et al) … but then a higher quality 2021 trial gave that a thumbs down as well (Liu).
Magnesium is likely not even relevant to exercise-induced cramps (Schwellnus). The whole idea has never been and is still “not supported by scientific evidence” (Minetto et al).
This evidence is a thin mix of good and bad news, maybe leaning a bit to the negative side. We know enough to know that magnesium will clearly not do the job for many people, but we also don’t fully understand the intricate physiology. Anyone with chronic pain should give it a shot — not because it’s super promising, but because it’s easy, cheap, and safe to experiment. This is just like the risk/benefit equation for vitamin D supplementation for pain: a harmless, non-crazy option for more desperate patients to try.
If I had neuropathy in particular, I’d probably start eating more salad. Especially potato salad! See dietary sources of magnesium.