Whacking joints “in” and sensation-enhanced placebo
David Butler of Noigroup in Australia has a terrific story about a client who brought him a gift of half a sheep. You should read the original — it’s just a good clinical yarn — but you can start with this highly condensed version and what I like about it. (It’s not really about sheep. That’s just a bit of memorable Australian colour.)
Fred was a middle-aged farmer with neck pain who believed he needed routine spinal “adjustments.” He specifically asked David to “whack them back in.” It wasn’t what David wanted to do for his patient! He knew that he had no good scientific justification for “whacking” anyone’s vertebrae “in”:
“I don’t think anything goes out except fires and me on occasional Friday nights. Joints may get a bit stiff or rarely, locked, but that is about it.”
Indeed, “spinal subluxation” is a controversial concept at best, and it’s unlikely that any spinal joint is ever dislocated such that it is literally “out” (without major trauma anyway).
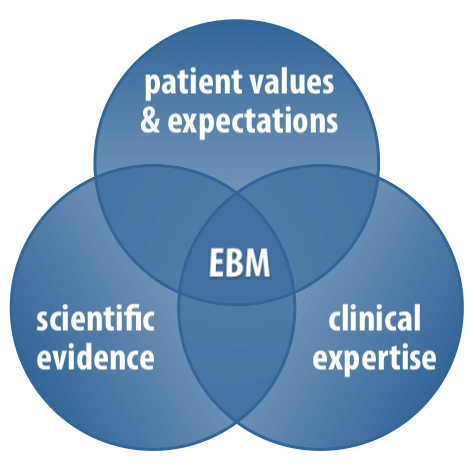
Nevertheless, David chose to do what Fred asked of him. Why? Because of one of the other pillars of evidence-based medicine: “patient values and expectations.”
And Fred wanted a whack, so Fred got whacked, and David got a happy customer … and a half sheep. 🙂
So what happened there? Anything?
Why was Fred satisfied, beyond just getting what he ordered? David says he “probably manipulated Fred’s perceptions as well as perhaps doing something to the joint structures,” but he clearly doesn’t think he did much to Fred’s joints. He calls it a placebo.
And that brings me to the bit I want to add: I think this was not just a good example of placebo, but of a sensation-enhanced placebo.
Sensation-enhanced placebo
Sensations are a uniquely potent way to satisfy patient expectations.
Most placebo uses a variety of psychological tactics to get the patients' hopes up, everything from just straight-up lying — “this is powerful medicine, it will heal you” — to infamously odd cues and clues like the colour of a pill. But you can take this to another level if you can induce a vivid sensation that makes the treatment seem like it’s really doing something, strongly reinforcing the patient’s beliefs about what is wrong and what will help it.
It’s one thing to think that the “medicine” is doing something. It’s another to feel it doing something.
I reckon sensation-enhanced placebo is the engine that powers most manual therapies — it’s actually the main reason they exist. For better or worse, this is why patients love to be massaged, adjusted, stretched, jostled and vibrated, taped and scraped, zapped and jabbed. And more. Read more about the concept of a “sensation-enhanced placebo.”
There is a members-only audio version of this post. You are a logged-in member — welcome! Download the 7MB MP3 file.
I will be improving audio delivery ASAP, but for now I’m just going to keep using this dirt simple method, because it gets the job done — and it just wouldn’t get done if I had to start a podcast first.
iPhone users: Please note that iPhones don’t handle downloaded audio files gracefully, but they definitely can play them. If you aren’t offered a sensible option to open and play the downloaded file in a suitable app, just go to the “Files” app — you can just play it directly from there, easy peasy.