Psoas, So What?
Massage therapy for the psoas major and iliacus (iliopsoas) muscles is not that big a deal
Two large hip flexor muscles are given unusual emphasis by many massage therapists and chiropractors. The popularity of psoas “work” — usually meaning both the psoas major muscle and iliacus muscle — is partly due to hype and mystique, and partly because it can be helpful at times (like massaging nearly any muscle can be).
Both patients and therapists need to consider whether it’s really necessary, however — psoas work is an uncomfortable, time-consuming, and expensive treatment to experiment with. It hits all three of the major red flags for quackery: potentially dangerous, distracting from better options, and a dubious rationale.
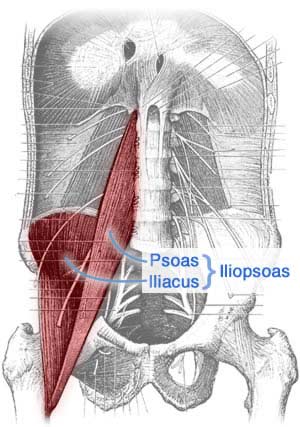
“Psoas” is oddly pronounced “so ass.” The iliopsoas “muscle” is actually two muscles that merge in the pelvis, the iliacus muscle & the psoas major muscle. You’ll rarely hear “iliacus” in the wild. Professionals usually refer to “the psoas” or “iliopsoas.”
That psoas mystique
Some have called it “the muscle of the soul.” So deep! So mysterious! So core! Pso-ass!
Iliopsoas massage is often pretentiously called psoas “work” — as in, “let’s do some psoas work today.” It implies something more profound and productive than mere massage. It’s just massage, and I dislike the “work” thing as much as I hate it when therapists call themselves “healers.”
But the mystique of iliopsoas massage is mostly due to simple geography: it’s just a tricky muscle to get to. The mechanics can defeat therapists, and the sensations can be rough for the patient.
It can be hard to even find iliopsoas if you don’t know exactly what you’re looking for, and many massage therapists with minimal training don’t know the anatomy even in the abstract, let alone how to tell the difference between the abdominal structures under their fingertips. True story: a well-trained therapist once confidently told me, “I’ve reached your psoas, and it’s really tight,” when she was actually, definitely just pressing on my spine. Things went downhill from there.1
It can also be a physically difficult muscle to get to even when you know just where to press — nearly all of it is hidden behind a wall of abs and guts. It’s easier to get to than you might think, considering its location, but much depends on the patient’s build. In slender people with a prominent lumbar curve, it can be almost effortless. Thicker people with less lordosis are a completely different story, and the psoas is out of reach in some heavy patients.
And it is possible to rip a hole in your intestines with abdominal massage.2 Admittedly unlikely if any reasonable amount of care is being taken, but possible. And not everyone takes a reasonable amount of care: see the appendix about the trend of standing on people’s guts to reach the psoas.
I can’t think of a muscle, other than the levator ani, that brings out the crazies like the psoas.
Facebook comment
Psoas sensitivity
The other big challenge is sensory: psoas massage is usually unpleasant. The iliopsoas seems to be quite sensitive to pressure — not to mention the tissues overlying it — and the quality of pain is almost always unpleasant. It takes time and caution to do it well and without causing significant discomfort. For many people, it’s just too much massage pressure.
What is easy is for everyone involved to fool themselves into thinking that the treatment is important simply because it’s so uncomfortable. Anything that hurts that much must be important and effective, right? A sensitive iliopsoas might need therapy, but you can’t assume that just because it feels bad. Even a happy, healthy psoas may feel quite sensitive. It can be uncomfortable regardless of whether it makes one bit of difference clinically.
The Psoas Book (is ridiculous)
Published in 1997, the year I started massage therapy college, The Psoas Book by Liz Koch3 is an influential, but short and amateurish hagiography4 of the psoas muscle. Every sentence oozes credulous enthusiasm and hyperbole about the profound clinical and emotional importance of the iliopsoas muscle. Example:
[The psoas] affects every facet of your life, from your physical well-being to who you feel yourself to be and how you relate to the world. A bridge linking the trunk to the legs, the psoas is critical for balanced alignment, proper joint rotation, and full muscular range of motion. … Whether you suffer from a sore back or anxiety, from knee strain or exhaustion, there’s a good chance that a constricted psoas muscle might be contributing to your woes.
Liz Koch, The psoas book, 1997
The mystique of the psoas has come entirely from this gushing, ridiculous book. It’s Liz Koch’s fault.
That goofy legacy is perpetuated today by many articles that pile on with fresh hyperbole, like this one on “TheMindUnleashed.com”: The ‘Muscle of the Soul’ may be Triggering Your Fear and Anxiety. This is a mind-bogglingly dumb article, but it’s extremely popular among massage therapists on Facebook, where they promoted it on an absurd scale — 135,000 likes and counting. That is a lot of foolish people. They are all probably huge fans of Ancient Aliens, too.5 Despite progress, the profession of massage therapy still richly deserves its flaky reputation, and practitioners do and say some extremely strange things.6

For instance, here’s a startlingly extreme example of fetishization of the psoas:
It so happens my sister was not only a young MD at the time, but also a physiatrist and very much into Dr. Travell. I read and reread Travell’s books (I still have boxes of photocopies of sections of her books) searching for the magic point or points to work on. I spent hours upon hours in the medical library. (I have a degree in engineering — I can read things technical and will dig in until I understand.) I rolled on tennis balls and lacrosse balls. I did the cooling sprays. I got needled and injected. I even visited a doctor in NYC who used a crazy long hat pin like needle to poke me deep in the psoas muscle. (In retrospect I am lucky that did not really mess me up.)
What could possibly go wrong?
Psoas massage is over-rated
Psoas massage is over-rated because it just isn’t needed for most people, most of the time. (Many people would argue that it is never needed, and they might be right.) Thanks to professional folklore and a tradition of psoas evangelism, most massage therapists and many chiropractors believe that the psoas is the missing piece in a biomechanical puzzle, particularly for back pain patients. This is a classic example of “structuralism”: the excessive focus on specific biomechanical origins of pain, especially ones that suggest marketable solutions.7 The message to patients is: “I can treat your back pain, because I understand how important the psoas is, unlike therapists with less insight into the intricate workings of the human body.”
No one actually has the faintest clue or evidence that the psoas is truly the key to back pain or anything else. It’s just another spinal muscle, no more or less important than any other. Unless you’re keen on core stability (and all psoas worshippers are), in which case it is less important than other muscles in the area, like the quadratus lumborum — the quadratus lumborum is actually “a better stabilizer of the spine than psoas,”8 and more accessible to and worthy of massage attention (see Massage Therapy for Low Back Pain).
There is no reason to emphasize it. If anything, there are great reasons not to. In particular, there doesn’t seem to be much of a relationship between tight psoas muscles and back pain, if any.910
Professionals should bear in mind that most patients consider any therapy — even pleasant, luxury therapy — to be a major and regrettable expense. Many patients can barely afford three appointments, and therapy should always be pragmatic and as efficient as possible, with a strict focus on doing only what is the most strongly indicated: bang for buck is critical. All other things being equal, always choose the cheapest and safest treatment option for your pain problem. It doesn’t matter that a few of those patients might benefit from a little psoas work — what matters is that most of them don’t need it enough to bother.
As a therapist, my attitude towards psoas was always “only suggest psoas work to my patient if we’re out of other options, and they’re still desperate, and we have some clear and specific reason to believe that it might make a difference.” Many other therapists take quite a different attitude: “Psoas is the secret to life itself: massage it first and strongly for $80/hour, or all is lost.” Psoas is a bit of a religion for those therapists. But that attitude is rarely a good idea.
In my opinion, it’s merely an interesting muscle, occasionally important … but usually just over-rated.
Guts are not for standing
In early 2015, this article made the rounds on social media: “SERIOUS WARNING – If you do any releases to your Psoas or Abs, you MUST READ THIS.” I don’t care for the article, and I’m not recommending it … but I sure do agree with its main point: it is indeed a “disturbing trend” that coaches and trainers are “helping people release by stepping on them,” including stepping on abdomens to target the iliopsoas muscle. I wasn’t aware that this was happening. If it actually is, it’s insane — the apotheosis of psoas hype. Sadly, I don’t have much trouble believing it.
Recall that is possible to severely damage your intestines with strong massage, as mentioned earlier (see Mori et al.).
The article is mainly a cautionary tale of an appendix rupture, which may well have been caused by amateurish, aggressive “release” of the psoas:
Karin told me she saw someone last week twice and during that time there were lots of “adjustments” and her “Psoas” was released fairly aggressively (Karin’s description)… [she] felt unwell after the session and got worse, such that she threw up twice within half an hour. She tried to put up with it (she is a tough girl) but couldn’t get any sleep that night and every time she moved, she had severe pain. She still had the vomiting and now diarrhea. When she contacted me, I told her to go straight to emergency as I thought she had a ruptured appendix.
Basically, she did.
When they operated on her, they took it out and found it had a small rupture in it.
Now, it could be that it was ready to go and a sneeze could have set it off but she had this pain since straight after the treatment and it only got worse. That is part of the risk of working in the abdomen – whether it is Psoas or Iliacus or whatever deep structure you are going for. There is a lot going on in there.
The article is poorly written and full of sloppy clinical reasoning, and all the vague talk about releasing muscles — as if that’s actually a meaningful clinical concept — grated on my nerves so badly it was hard to get through the piece.
But these are quibbles. The main point is sound. Standing on guts to release the psoas muscle is a Very Bad Idea.
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
What’s new in this article?
2020 — Minor additions, mainly a startlingly extreme example of fetishization of the psoas.
2020 — Added reference to a case study of severe injury from deep abdominal massage.
2017 — Added a citation that strongly emphasizes that psoas is not critical to core stability.
2010 — Publication.
Notes
- “That’s my spine,” I said. She moved a bit to the left, “Ah, there we go, I think I have it now.” But no! “Now you’re pressing on my aorta,” I said. “Can’t you feel the pulse?” Her eyes widened: “Is that your pulse?” What the hell else would it be? I thought. Within another minute, I had guided her to the muscle belly, demonstrated how it pops out with slight hip flexion, and she was fine from there on. But her initial difficulty emphasizes that this is awkward palpation work. You’re groping around in guts.
- Mori S, Ai T, Otomo Y. Laceration of the transverse mesocolon in an old man with a habit of abdominal massage for constipation: a case report. Surg Case Rep. 2020 Jan;6(1):1. PubMed 31898753 ❐ PainSci Bibliography 52515 ❐
This is a description of a case of intestinal injury following self-massage of the abdomen intended to help constipation. A 68-year-old man with chronic constipation had a habit of abdominal self-massage, and “did it hard” shortly before developing severe belly pain. He was misdiagnosed with a tumour at the hospital. A day later, still bleeding internally, a surgeon found a litre and a half of blood and a five centimetre tear in his upper colon. The patient recovered surprisingly well after an imperfect repair — the intestinal tissue was too fragile to stitch the tear closed properly. His only complication was an ironic increase in constipation from a paralyzed intestine. When traumatized, the intestine stops contracting for safety.
The authors of the report reasonably assume that the injury was caused by the self-massage, but note other possible explanations, “such as rupture of small aneurysms.” However, the lesion was quite a bit too large to be explained by anything but the most obvious.
- Koch L. The psoas book. Guinea Pig; 1997.
- One of my favourite obscure words. Strictly speaking, a hagiography is a biography of a saint or ecclesiastical celebrity. However, it’s also “a pejorative reference to the works of biographers and historians perceived to be uncritical or reverential to their subject,” and this is arguably the more common usage in a non-specialist context.
- If you think Ancient Aliens is legit, you’re probably beyond hope, but perhaps you can still be salvaged if you watch Ancient Aliens Debunked.
- Ingraham. 💩 Massage Therapists Say: A compilation of more than 50 examples of the bizarre nonsense spoken by massage therapists with delusions of medical knowledge. PainScience.com. 11683 words.
- Ingraham. Your Back Is Not Out of Alignment: Debunking the obsession with alignment, posture, and other biomechanical bogeymen as major causes of pain. PainScience.com. 21878 words.
- McGill S, Juker D, Kropf P. Quantitative intramuscular myoelectric activity of quadratus lumborum during a wide variety of tasks. Clin Biomech (Bristol, Avon). 1996 Apr;11(3):170–172. PubMed 11415616 ❐ “Electromyographic evidence, together with architectural features make the quadratus lumborum a better stabilizer of the spine than psoas. Use of horizontal ‘side support’ exercise to train this muscle would appear to be a wise choice.”
- Hellsing AL. Tightness of hamstring and psoas major muscles: A prospective study of back pain in young men during their military service. Ups J Med Sci. 1988;93(3):267–76. PubMed 2977003 ❐
From the abstract: “Tight hamstring- or psoas muscles could not be shown to correlate to current back pain or to the incidence of back pain during the follow-up period.”
- Nourbakhsh MR, Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther. 2002 Sep;32(9):447–60. PubMed 12322811 ❐
The key findings:
“It appears that muscle endurance and weakness are associated with LBP and that structural factors such as the size of the lumbar lordosis, pelvic tilt, leg length discrepancy, and the length of abdominal, hamstring, and iliopsoas muscles are not associated with the occurrence of LBP.”
Nourbakhs and Arab did indeed identify a correlation between cLBP and pain and poor muscle endurance and strength, but correlation is (famously) not causation. They did not establish that the relationship is causal, or that improving these metrics is therapeutic, so note that their data is not very useful for supporting the value of core training as an intervention for back pain. And so, despite finding weak back muscles in back pain patients, it cannot by itself support the value of core training (meanwhile, there's a bunch of other more relevant and recent evidence to consider).
What I think is most significant in their results is that found not even a correlation between chronic low back pain and various "structural" features. And where there is not even a correlation, there cannot be causation! So this data is useful for supporting the point that structure doesn't seem to have much to do with back pain.
